Understanding Fatigue: When Is It More Than Just Being Tired?
Fatigue is a common experience that everyone encounters at some point in their lives. It can result from a variety of factors, including lack of sleep, poor nutrition, or simply a busy lifestyle. However, when fatigue becomes persistent, overwhelming, or unexplained, it may be more than just an everyday occurrence. Understanding when fatigue could be indicative of a deeper health issue, such as a heart problem, is crucial for taking timely action.
Fatigue associated with heart problems often presents differently than general tiredness. It can feel more intense, long-lasting, and may not improve with rest or sleep. Recognizing the signs that differentiate ordinary fatigue from heart-related fatigue is essential for early diagnosis and management of potential heart conditions. By identifying these warning signs, individuals can seek medical advice promptly and take steps to improve their heart health.
 When Fatigue is a Sign of a Heart Problem
When Fatigue is a Sign of a Heart Problem
- Fatigue that persists despite adequate rest and sleep
- Excessive tiredness that interferes with daily activities
- Fatigue accompanied by other symptoms like shortness of breath or chest pain
The Connection Between Fatigue and Heart Health
Fatigue can be a complex symptom that is often linked to various health conditions, including those affecting the heart. When the heart is unable to pump blood efficiently, the body’s organs and tissues may not receive the necessary oxygen and nutrients they need to function properly. This can lead to a sense of overwhelming tiredness, as the body struggles to meet its energy demands. Understanding the connection between fatigue and heart health is crucial for recognizing potential heart problems early.
Heart-related fatigue is typically characterized by a lack of energy that doesn’t improve with rest, and it may occur alongside other symptoms such as shortness of breath, chest discomfort, or an irregular heartbeat. It’s not just about feeling tired; it’s about feeling an intense lack of energy that disrupts daily life. Individuals experiencing this type of fatigue should be vigilant and consider seeking medical advice to rule out or confirm a heart condition.
 When Fatigue is a Sign of a Heart Problem
When Fatigue is a Sign of a Heart Problem
How the Heart Affects Energy Levels
The heart plays a central role in maintaining the body’s energy levels by supplying oxygen-rich blood to every part of the body. When the heart’s function is compromised, it affects the body’s ability to sustain normal energy levels. Conditions such as heart failure, coronary artery disease, and arrhythmias can impede blood flow, leading to reduced oxygen delivery and, consequently, fatigue.
For example, heart failure occurs when the heart cannot pump blood efficiently, leading to congestion in the lungs and other parts of the body. This reduces oxygenation and can cause severe fatigue. Similarly, coronary artery disease narrows the arteries that supply blood to the heart muscle, limiting the heart’s ability to function optimally and often resulting in fatigue as a symptom.
- Heart failure: Reduced pumping capacity of the heart leading to fatigue
- Coronary artery disease: Narrowing of arteries causing limited blood flow and tiredness
- Arrhythmias: Irregular heartbeats affecting blood circulation and energy levels
Symptoms to Watch For Alongside Fatigue
While fatigue can be an important sign of a heart problem, it rarely occurs in isolation. Often, it is accompanied by other symptoms that, when present together, provide a clearer picture of a potential heart issue. Recognizing these accompanying symptoms can help in differentiating heart-related fatigue from general tiredness and prompt timely medical evaluation.
 When Fatigue is a Sign of a Heart Problem
When Fatigue is a Sign of a Heart Problem
Shortness of Breath
Shortness of breath, especially during physical activity or when lying down, is a common symptom associated with heart problems. This occurs when the heart cannot pump blood effectively, leading to fluid build-up in the lungs. This makes it difficult for oxygen to enter the bloodstream, causing breathlessness even with minimal exertion. If you find yourself easily winded or struggling to catch your breath, especially when it is coupled with fatigue, it is essential to consult a healthcare provider.
Chest Pain or Discomfort
Chest pain, pressure, or discomfort is one of the hallmark signs of heart issues. This symptom, often referred to as angina, occurs when the heart muscle doesn’t receive enough blood flow, usually due to narrowed arteries. While not all chest pain is heart-related, if it occurs alongside fatigue, it can be a significant warning sign of a heart condition such as coronary artery disease. This pain might feel like a squeezing, fullness, or sharp sensation that spreads to the neck, jaw, or arms.
Irregular Heartbeat
An irregular heartbeat, or arrhythmia, can also accompany fatigue. Arrhythmias occur when the electrical impulses that coordinate heartbeats don’t work properly, causing the heart to beat too fast, too slow, or erratically. This irregularity can lead to inefficient blood flow, reducing the amount of oxygen circulating throughout the body and resulting in fatigue. Symptoms like palpitations, dizziness, or feeling lightheaded in addition to fatigue could indicate an underlying heart rhythm problem.
- Shortness of breath during daily activities or rest
- Chest discomfort that spreads to other areas of the upper body
- Irregular or rapid heartbeats, often felt as palpitations
Diagnosing Heart-Related Fatigue: What to Expect
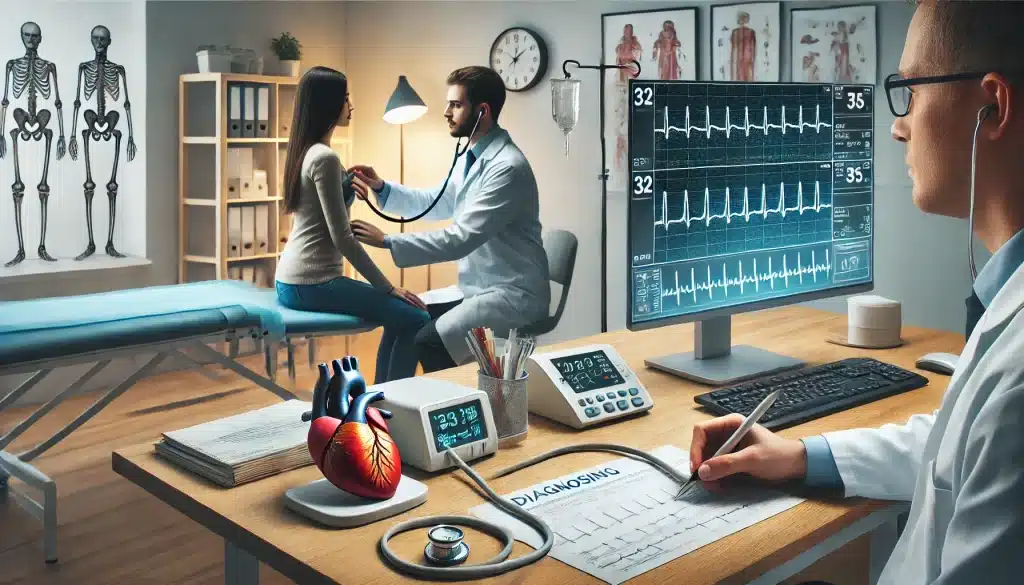
If you suspect that your fatigue may be linked to a heart problem, it is important to seek medical evaluation. Diagnosing heart-related fatigue involves a thorough assessment by a healthcare provider, who will consider your symptoms, medical history, and risk factors. The diagnostic process aims to determine whether the fatigue is indeed related to a heart condition or if other underlying issues may be at play.
 When Fatigue is a Sign of a Heart Problem
When Fatigue is a Sign of a Heart Problem
Medical Tests and Evaluations
Your healthcare provider will likely start with a physical examination and ask detailed questions about your fatigue and any accompanying symptoms. They may check your heart rate, blood pressure, and listen for any unusual sounds in your heart or lungs. Depending on the initial findings, further tests may be recommended to assess your heart health in more detail.
Common tests used to diagnose heart-related fatigue include:
- Electrocardiogram (ECG): This test records the electrical activity of the heart and can help identify irregular heart rhythms or other abnormalities.
- Echocardiogram: An ultrasound of the heart that provides images of heart structure and function, helping to detect problems with the heart’s valves, chambers, or pumping strength.
- Stress Test: This test measures how your heart performs under physical stress, typically through exercise or medication that simulates exercise effects.
- Blood Tests: Tests such as a complete blood count (CBC) or checks for markers of heart failure can provide insight into whether your fatigue is heart-related.
- Coronary Angiography: A procedure that uses contrast dye and X-rays to view the blood flow through your coronary arteries, identifying blockages or narrowing that could be causing fatigue.
Working with Your Healthcare Provider
Open communication with your healthcare provider is key to effectively diagnosing and managing heart-related fatigue. Be prepared to discuss your symptoms in detail, including when they started, their severity, and any factors that seem to worsen or improve them. Your provider may also ask about your lifestyle, diet, physical activity levels, and any family history of heart disease.
It’s important to follow your provider’s recommendations for further testing or treatment and to keep track of your symptoms over time. Early diagnosis and intervention can make a significant difference in managing heart-related fatigue and improving overall heart health.
Managing Fatigue Related to Heart Problems
Once a heart-related cause of fatigue has been identified, managing the condition involves a combination of lifestyle changes, medical treatments, and ongoing monitoring. Effective management aims not only to alleviate fatigue but also to address the underlying heart condition, improve quality of life, and prevent further complications. Here are some strategies that can help manage fatigue related to heart problems.
 When Fatigue is a Sign of a Heart Problem
When Fatigue is a Sign of a Heart Problem
Lifestyle Changes for Improved Energy
Adopting a heart-healthy lifestyle is one of the most effective ways to manage fatigue. This includes maintaining a balanced diet, regular physical activity, adequate sleep, and stress management. Diets rich in fruits, vegetables, whole grains, lean proteins, and healthy fats support overall cardiovascular health and energy levels. Reducing intake of processed foods, sugars, and saturated fats can also help in managing fatigue.
Regular physical activity, tailored to your condition and capabilities, can improve heart function and overall energy. Activities such as walking, swimming, or light aerobic exercises can enhance cardiovascular endurance and reduce fatigue. However, it’s important to consult with a healthcare provider before starting any exercise regimen, as certain heart conditions may require specific precautions.
Medications and Treatments
Depending on the specific heart condition diagnosed, medications may be prescribed to manage symptoms and improve heart function. Common medications include:
- Beta-blockers: Help reduce heart rate and lower blood pressure, easing the heart’s workload and reducing fatigue.
- ACE inhibitors: Help relax blood vessels, improve blood flow, and reduce the strain on the heart.
- Diuretics: Help remove excess fluid from the body, reducing swelling and shortness of breath, which can improve energy levels.
- Anti-arrhythmic drugs: Help control irregular heart rhythms, improving the efficiency of the heart’s pumping action.
In some cases, surgical interventions may be necessary to address the underlying heart condition, such as coronary artery bypass grafting (CABG) for blocked arteries or valve repair or replacement surgeries. Ongoing monitoring and regular follow-ups with your healthcare provider are essential to track progress and adjust treatments as needed.
Additional Tips for Managing Fatigue
- Prioritize activities and conserve energy for essential tasks.
- Break tasks into smaller, manageable steps and take breaks as needed.
- Maintain a regular sleep schedule to improve rest and recovery.
- Stay hydrated and avoid excessive caffeine or alcohol, which can affect sleep and energy levels.
Preventive Measures: Reducing Your Risk of Heart-Related Fatigue
Preventing heart-related fatigue involves proactive steps to maintain heart health and reduce the risk of cardiovascular conditions. By making conscious lifestyle choices and managing risk factors, individuals can improve their overall well-being and reduce the likelihood of experiencing fatigue due to heart problems. Here are some key preventive measures to consider:
 When Fatigue is a Sign of a Heart Problem
When Fatigue is a Sign of a Heart Problem
Importance of Regular Exercise and Diet
Regular exercise is a cornerstone of heart health. Engaging in at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, cycling, or swimming, can strengthen the heart, improve circulation, and boost overall energy levels. Strength training exercises at least two days a week can also contribute to improved cardiovascular fitness and muscle endurance.
Alongside exercise, a heart-healthy diet plays a critical role in preventing heart-related fatigue. Focus on incorporating a variety of nutrient-dense foods, including:
- Fruits and vegetables: Rich in vitamins, minerals, and antioxidants that support heart health.
- Whole grains: Provide essential fiber that helps regulate cholesterol and blood pressure.
- Lean proteins: Such as fish, poultry, and legumes, which support muscle function without adding excess fat.
- Healthy fats: Found in nuts, seeds, avocados, and olive oil, which can help reduce inflammation and improve cholesterol levels.
Avoid excessive intake of sodium, sugars, and trans fats, which can contribute to high blood pressure, obesity, and other heart disease risk factors. Maintaining a balanced diet not only supports heart health but also helps maintain energy levels and prevent fatigue.
Monitoring Heart Health
Regular monitoring of heart health is essential, especially for individuals with risk factors such as high blood pressure, high cholesterol, diabetes, or a family history of heart disease. Regular check-ups with a healthcare provider, including routine blood tests and heart screenings, can help detect potential issues early and allow for timely intervention.
Monitoring should include:
- Blood pressure: Keep blood pressure within normal ranges to reduce the strain on the heart.
- Cholesterol levels: Manage cholesterol through diet, exercise, and medications if necessary to prevent artery blockages.
- Blood sugar levels: Controlling blood sugar helps reduce the risk of diabetes-related heart complications.
- Body weight: Maintaining a healthy weight reduces the burden on the heart and lowers the risk of heart disease.
Additionally, managing stress, avoiding smoking, and limiting alcohol intake are critical components of heart health. These preventive measures, combined with regular medical evaluations, can significantly reduce the risk of heart-related fatigue and improve overall quality of life.
FAQs About Fatigue and Heart Problems
Can fatigue be the only sign of a heart problem?
Yes, fatigue can sometimes be the only noticeable symptom of a heart problem, especially in the early stages. Unlike more obvious signs like chest pain or shortness of breath, fatigue may be subtle and easily overlooked. However, if fatigue is persistent, unexplained, and interferes with your daily activities, it is important to consult with a healthcare provider to rule out any underlying heart conditions.
How can I tell if my fatigue is heart-related?
Determining if your fatigue is heart-related involves paying attention to additional symptoms such as shortness of breath, chest discomfort, or palpitations. If your fatigue is accompanied by these or other signs of heart distress, it could indicate a cardiovascular issue. A medical evaluation, including a detailed history, physical examination, and diagnostic tests like an ECG or echocardiogram, can help identify whether your fatigue is due to a heart problem.
What should I do if I suspect my fatigue is heart-related?
If you suspect your fatigue may be related to a heart problem, the first step is to schedule an appointment with your healthcare provider. They will assess your symptoms, conduct necessary tests, and provide a diagnosis. Early detection and intervention are crucial for managing heart-related fatigue effectively. In the meantime, keep track of your symptoms, avoid strenuous activities, and follow any preliminary advice your provider may have given you about managing fatigue and heart health.