Understanding Recurring Chest Pain
Recurring chest pain can be alarming and may indicate an underlying health condition that requires attention. It is essential to understand that chest pain does not always stem from heart problems; it can be caused by various factors, including gastrointestinal, musculoskeletal, or even psychological issues. Recognizing the nature and triggers of your chest pain is the first step toward effective prevention and management.
Chest pain may present itself in different forms, such as a sharp stabbing sensation, a dull ache, or even a burning feeling. The pain can vary in intensity, duration, and frequency, making it challenging to pinpoint the exact cause without professional evaluation. Therefore, it is crucial to take recurring chest pain seriously and consult a healthcare provider for an accurate diagnosis and appropriate treatment.
- Understanding your pain patterns and triggers is essential.
- Professional medical evaluation is recommended for accurate diagnosis.
- Not all chest pain is heart-related; other systems can be involved.
Common Causes of Recurring Chest Pain
Identifying the root causes of recurring chest pain is crucial in developing an effective prevention strategy. Chest pain can originate from various body systems, each presenting distinct characteristics and implications. Below, we explore the most common causes, categorizing them into cardiovascular, gastrointestinal, and musculoskeletal origins.
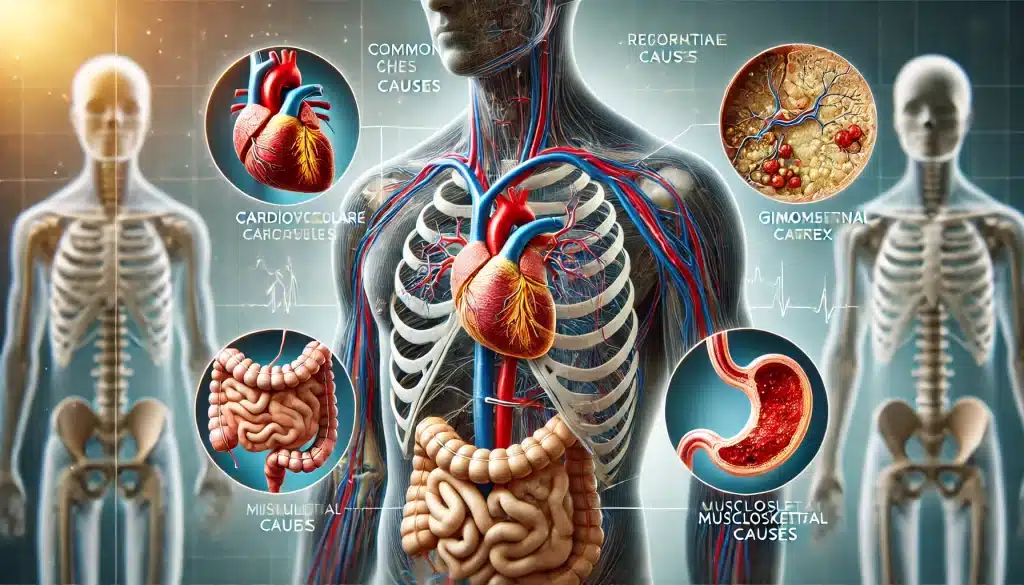
Cardiovascular Causes
Cardiovascular issues are often the first consideration when it comes to chest pain. Conditions such as angina, which occurs when the heart muscle doesn’t get enough oxygen-rich blood, can cause recurrent pain, especially during physical exertion or emotional stress. Another common cause is myocardial infarction, or a heart attack, which is a medical emergency that requires immediate attention. Other cardiovascular conditions, like pericarditis (inflammation of the lining around the heart) and aortic dissection, can also lead to recurring chest pain.
- Angina: Pain due to reduced blood flow to the heart.
- Myocardial infarction: Commonly known as a heart attack.
- Pericarditis: Inflammation of the pericardium, the sac surrounding the heart.
Gastrointestinal Causes
Gastrointestinal problems are another significant source of chest pain. Acid reflux, or gastroesophageal reflux disease (GERD), can cause a burning sensation in the chest known as heartburn. This pain often occurs after eating and can be exacerbated by lying down or bending over. Esophageal spasms, which are abnormal contractions of the muscles in the esophagus, can also mimic heart pain. In some cases, a hiatal hernia, where part of the stomach pushes up into the chest cavity, can lead to discomfort and recurring chest pain.
- Acid reflux (GERD): Causes heartburn and chest pain.
- Esophageal spasms: Can mimic heart-related chest pain.
- Hiatal hernia: Part of the stomach protrudes into the chest area.
Musculoskeletal Causes
Musculoskeletal causes of chest pain involve the muscles, bones, and nerves in the chest area. Costochondritis, an inflammation of the cartilage that connects the ribs to the breastbone, is a common culprit of recurring chest pain. This type of pain is often sharp and worsens with movement or pressure on the affected area. Muscle strains, injuries, and even prolonged poor posture can also contribute to musculoskeletal chest pain, making it essential to distinguish these sources from more serious conditions.
- Costochondritis: Inflammation of rib cartilage causing sharp pain.
- Muscle strains: Resulting from overuse or injury.
- Poor posture: Can lead to musculoskeletal discomfort in the chest.
Risk Factors for Recurring Chest Pain
Understanding the risk factors associated with recurring chest pain can help in taking proactive measures to reduce the frequency and severity of the episodes. Risk factors can be broadly divided into lifestyle factors and medical conditions, each playing a significant role in the development and persistence of chest pain.
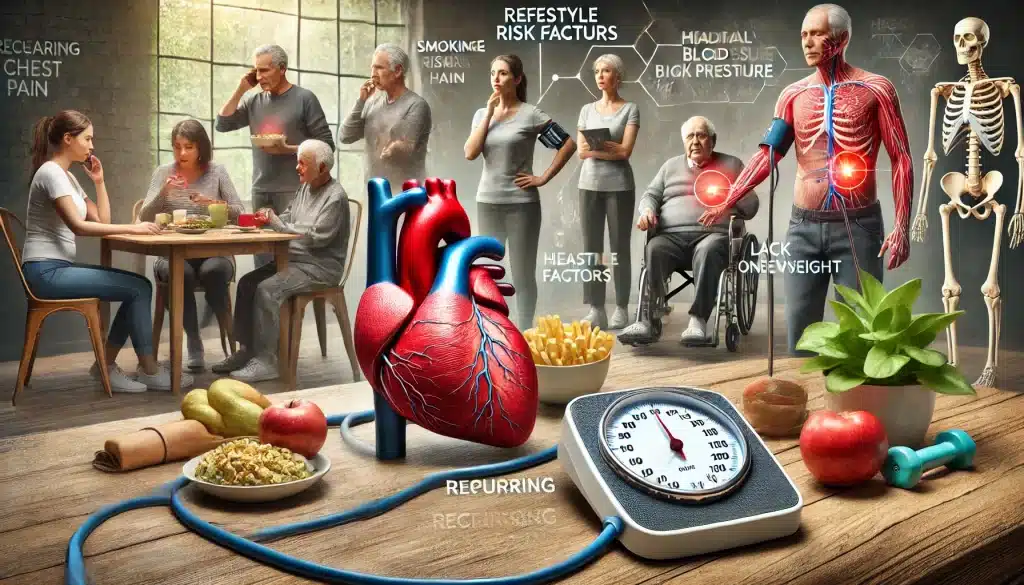
Lifestyle Factors
Certain lifestyle habits significantly increase the risk of experiencing recurring chest pain. Smoking, for example, not only damages the lungs but also affects the cardiovascular system, leading to conditions like angina or even a heart attack. A sedentary lifestyle, characterized by prolonged inactivity and lack of exercise, can contribute to obesity and poor cardiovascular health, increasing the likelihood of chest pain. Unhealthy dietary choices, such as high consumption of fatty, sugary, and processed foods, can exacerbate conditions like acid reflux and contribute to cardiovascular problems.
- Smoking: Increases cardiovascular risks and damages lung health.
- Sedentary lifestyle: Lack of exercise leads to poor heart health.
- Unhealthy diet: Contributes to acid reflux and cardiovascular issues.
Medical Conditions
Several medical conditions are known to predispose individuals to recurring chest pain. Coronary artery disease (CAD) is one of the most common, where the arteries supplying blood to the heart become narrowed or blocked, leading to chest pain, especially during physical activity. Hypertension, or high blood pressure, can strain the heart and lead to angina. Additionally, individuals with anxiety disorders may experience chest pain as a symptom of panic attacks, which, while not directly harmful to the heart, can be distressing and mimic heart-related pain.
- Coronary artery disease (CAD): Narrowed arteries cause chest pain.
- Hypertension: High blood pressure increases strain on the heart.
- Anxiety disorders: Can cause chest pain during panic attacks.
Symptoms to Watch Out For
Recurring chest pain can present in various ways, and understanding the associated symptoms is crucial for timely intervention and management. Recognizing when chest pain is a sign of something serious, like a heart attack, or when it might be related to less urgent issues, like acid reflux, can make a significant difference in outcomes. Here are the key symptoms to be aware of when dealing with recurring chest pain:

When to Seek Immediate Medical Attention
Chest pain that occurs suddenly and is severe, crushing, or accompanied by other symptoms such as shortness of breath, sweating, nausea, or pain radiating to the jaw, neck, or arm, should be treated as a medical emergency. These symptoms may indicate a heart attack or other life-threatening conditions that require immediate medical intervention. Additionally, chest pain that is persistent, worsening, or does not improve with rest should prompt urgent evaluation by a healthcare provider.
- Severe or crushing chest pain: Could indicate a heart attack.
- Accompanied symptoms: Shortness of breath, sweating, nausea.
- Pain radiating: To the jaw, neck, or arm.
Other symptoms to watch for include dizziness, lightheadedness, or fainting episodes associated with chest pain, as these can be signs of a serious cardiovascular issue. Pain that worsens with exertion and improves with rest could also suggest angina. Conversely, pain that varies with body position or breathing might indicate a non-cardiac cause, such as a musculoskeletal or pulmonary origin.
- Dizziness or fainting: Can indicate cardiovascular problems.
- Pain with exertion: Suggests angina.
- Variable pain: May suggest musculoskeletal or pulmonary causes.
Preventive Strategies for Recurring Chest Pain
Preventing recurring chest pain involves adopting a multifaceted approach that includes lifestyle modifications, dietary changes, stress management, and, in some cases, medical interventions. By implementing these strategies, individuals can reduce the frequency and intensity of chest pain episodes, improve overall health, and enhance quality of life.

Lifestyle Modifications
One of the most effective ways to prevent recurring chest pain is through lifestyle changes. Regular physical activity, such as walking, cycling, or swimming, can improve cardiovascular health, reduce stress, and help maintain a healthy weight. It is important to choose exercises that are appropriate for your fitness level and any underlying health conditions. Quitting smoking is another critical step, as it significantly reduces the risk of heart disease and other chest pain causes. Limiting alcohol intake and avoiding illicit drugs can also play a role in preventing chest pain.
- Regular exercise: Improves heart health and reduces stress.
- Quit smoking: Reduces the risk of heart disease and chest pain.
- Limit alcohol and avoid drugs: Helps prevent chest pain episodes.
Dietary Recommendations
Diet plays a significant role in preventing chest pain, especially when it is related to cardiovascular or gastrointestinal causes. A heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help manage weight, lower cholesterol levels, and reduce blood pressure. Avoiding foods high in saturated fats, trans fats, and excessive sugars is crucial. For those prone to acid reflux, eating smaller, more frequent meals and avoiding spicy, acidic, or fatty foods can prevent heartburn and chest pain. Staying hydrated and avoiding large meals before bedtime are also beneficial strategies.
- Heart-healthy diet: Includes fruits, vegetables, and whole grains.
- Avoid unhealthy fats and sugars: Reduces cardiovascular risks.
- Manage reflux: Smaller meals and avoid trigger foods.
Stress Management Techniques
Stress is a known trigger for chest pain, particularly for individuals with anxiety disorders or heart conditions. Learning to manage stress through relaxation techniques, such as deep breathing exercises, meditation, or yoga, can be highly effective. Engaging in hobbies, spending time with loved ones, and ensuring adequate sleep are also important for stress reduction. In some cases, seeking professional help from a therapist or counselor to address chronic stress or anxiety can make a significant difference in preventing chest pain.
- Relaxation techniques: Deep breathing, meditation, yoga.
- Engage in hobbies and social activities: Reduces stress levels.
- Professional help: Therapy or counseling for chronic stress or anxiety.
Medical Interventions for Prevention
In addition to lifestyle and dietary changes, medical interventions may be necessary for individuals experiencing recurring chest pain, especially when underlying medical conditions are involved. These interventions can range from medications to surgical options, depending on the cause and severity of the pain. Consulting with a healthcare provider is essential to determine the most appropriate treatment plan.

Medications
Several medications can be prescribed to help prevent recurring chest pain. For cardiovascular-related chest pain, such as angina, doctors may prescribe nitroglycerin to relieve pain or beta-blockers and calcium channel blockers to reduce heart workload and prevent pain episodes. Statins may be used to lower cholesterol levels, reducing the risk of coronary artery disease progression. For gastrointestinal causes, antacids, H2 blockers, or proton pump inhibitors may be recommended to control acid reflux and prevent heartburn-related chest pain. In cases of musculoskeletal pain, anti-inflammatory drugs or muscle relaxants may be prescribed.
- Nitroglycerin: Relieves angina-related chest pain.
- Beta-blockers and calcium channel blockers: Reduce heart workload.
- Statins: Lower cholesterol and reduce cardiovascular risks.
- Antacids and proton pump inhibitors: Control acid reflux.
Surgical Options
In some cases, surgical intervention may be required to address the underlying cause of recurring chest pain. For individuals with severe coronary artery disease, procedures like angioplasty, where a stent is placed to open up blocked arteries, can help improve blood flow and prevent chest pain. Coronary artery bypass grafting (CABG) is another option for patients with multiple blocked arteries, where blood flow is rerouted around the blockage. For gastrointestinal causes, surgical options might include procedures to correct a hiatal hernia or other structural abnormalities contributing to chest pain.
- Angioplasty: Opens blocked arteries to improve blood flow.
- Coronary artery bypass grafting (CABG): Reroutes blood around blocked arteries.
- Surgery for gastrointestinal causes: Corrects structural issues.
Regular Monitoring and Follow-up
Regular monitoring and follow-up care are critical components in the prevention of recurring chest pain. Ongoing assessment allows healthcare providers to track the effectiveness of the implemented strategies, make necessary adjustments, and promptly address any new or worsening symptoms. This proactive approach is especially important for individuals with chronic conditions that predispose them to chest pain.
Importance of Routine Check-ups
Routine check-ups with a healthcare provider play a vital role in managing and preventing recurring chest pain. These visits allow for the early detection of changes in health status that could increase the risk of chest pain, such as rising blood pressure, cholesterol levels, or signs of new cardiovascular issues. Regular check-ups also provide an opportunity for individuals to discuss any concerns or symptoms with their doctor, ensuring that their treatment plan remains effective and up-to-date. Preventive screenings, like stress tests or echocardiograms, may be recommended based on individual risk factors.
- Routine check-ups: Early detection of risk factors and health changes.
- Discuss symptoms: Keep the treatment plan effective.
- Preventive screenings: Stress tests, echocardiograms, as needed.
Diagnostic Tests and Procedures
To accurately monitor heart health and identify potential causes of chest pain, healthcare providers may recommend various diagnostic tests and procedures. Electrocardiograms (ECGs) are commonly used to assess heart rhythm and detect any abnormalities that might cause pain. Stress tests help evaluate how the heart performs under physical exertion, which can reveal problems not seen during rest. For more detailed imaging, coronary angiography or CT scans may be used to visualize blood vessels and detect blockages or other structural issues. Regular monitoring through these tests can help prevent recurring chest pain by catching issues early and adjusting treatment accordingly.
- Electrocardiograms (ECGs): Assess heart rhythm and detect abnormalities.
- Stress tests: Evaluate heart performance under exertion.
- Coronary angiography or CT scans: Visualize blood vessels and blockages.
Frequently Asked Questions (FAQ)
What should I do if I experience chest pain frequently?
If you experience chest pain frequently, it’s important to consult a healthcare provider to determine the underlying cause. They may recommend lifestyle changes, medications, or other interventions to help manage and prevent the pain. Do not ignore recurring chest pain, as it could be a sign of a serious condition.
Can stress cause recurring chest pain?
Yes, stress can cause recurring chest pain, particularly in individuals with anxiety disorders or those prone to panic attacks. Stress can also exacerbate existing conditions such as angina. Managing stress through relaxation techniques, regular exercise, and professional support can help reduce chest pain related to stress.
Are all chest pains heart-related?
No, not all chest pains are related to the heart. Chest pain can also originate from gastrointestinal issues like acid reflux, musculoskeletal problems such as costochondritis, or even psychological factors like anxiety. It is important to identify the specific cause of your chest pain to address it appropriately.
What lifestyle changes can help prevent chest pain?
Lifestyle changes that can help prevent chest pain include regular exercise, a healthy diet, quitting smoking, limiting alcohol intake, and managing stress. These changes improve overall heart health, reduce risk factors for cardiovascular disease, and can help manage other conditions that cause chest pain.
When should I seek emergency care for chest pain?
You should seek emergency care for chest pain if it is severe, sudden, or accompanied by symptoms such as shortness of breath, sweating, nausea, or pain radiating to your jaw, neck, or arm. These could be signs of a heart attack or other serious conditions that require immediate medical attention.


