Understanding Genetic Risk Factors for Heart Disease
Heart disease is influenced by a variety of factors, and genetics play a significant role in determining how prone a person may be to developing this condition. If heart disease runs in your family, it’s important to understand how genetic predisposition affects your risk. While lifestyle factors such as diet and exercise are vital for heart health, your genes can sometimes predispose you to certain conditions like high blood pressure or high cholesterol, which contribute to heart disease.
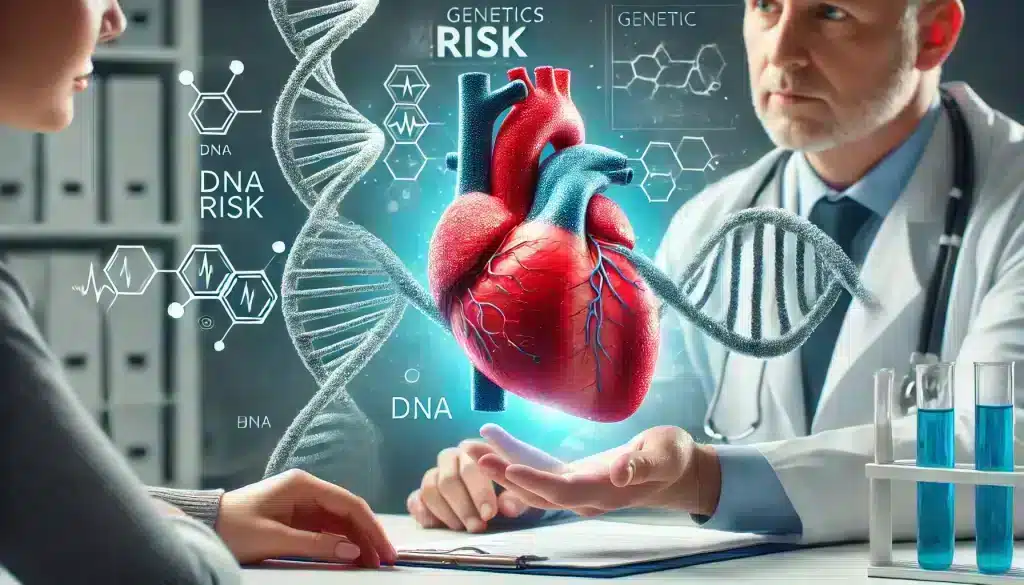
Inherited conditions, such as familial hypercholesterolemia, lead to elevated cholesterol levels that are often resistant to dietary and lifestyle changes alone. Individuals with this genetic condition are more likely to develop heart disease at an earlier age. However, identifying these risks early through genetic testing and family history can empower individuals to take proactive measures, reducing the overall risk of a heart attack or stroke.
How Genes Influence Heart Disease
Genes dictate many of the biological processes that regulate your heart’s health. Cholesterol metabolism, blood clotting, and blood pressure regulation are just a few examples of processes influenced by genetics. For example, specific gene mutations may cause your body to process cholesterol inefficiently, leading to plaque buildup in your arteries, which can increase the risk of heart disease.
Another example is inherited arrhythmias, where certain gene variants cause irregular heartbeats. These irregularities can strain the heart, increasing the risk of heart failure or sudden cardiac events. Understanding these genetic tendencies allows for targeted interventions, such as lifestyle modifications or medications, to mitigate the risk.
Table: Common Genetic Conditions Related to Heart Disease
| Condition | Description | Impact on Heart Disease |
|---|---|---|
| Familial Hypercholesterolemia | A genetic disorder characterized by high cholesterol levels from birth | Increases risk of coronary artery disease and heart attacks |
| Inherited Arrhythmias | Genetic mutations causing irregular heartbeats | Leads to heart failure or sudden cardiac events |
The Role of Lifestyle in Preventing Heart Disease
While genetics play a role in increasing the risk of heart disease, lifestyle choices have a significant impact on preventing its onset, even for those with a strong family history. Preventing heart disease family history is possible through consistent and deliberate actions focusing on diet, exercise, and stress management. Your daily habits can either enhance or diminish your heart health, making lifestyle changes essential for anyone at genetic risk.

Living a heart-healthy lifestyle can reduce the likelihood of developing heart disease by addressing key factors such as high blood pressure, cholesterol levels, and weight. By making healthier choices, you take control of the elements within your reach, minimizing the risk despite the genetic predispositions you may have inherited.
How a Heart-Healthy Diet Can Make a Difference
One of the most impactful lifestyle changes is adopting a heart-healthy diet. A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can significantly reduce the risk of heart disease. Foods that are high in saturated fats, sodium, and added sugars should be minimized as they contribute to high cholesterol, high blood pressure, and obesity, all of which increase heart disease risk.
Incorporating healthy fats like omega-3 fatty acids found in fish, nuts, and seeds can help lower cholesterol and reduce inflammation in the arteries. These dietary choices are critical in counteracting the potential impact of a genetic predisposition to heart disease.
Along with making smarter food choices, it’s essential to monitor portion sizes and caloric intake, especially for those who may have inherited metabolic conditions that lead to weight gain. Controlling weight is a vital part of preventing heart disease family history, and diet plays a major role in that.
Physical Activity: A Powerful Tool for Heart Disease Prevention
Regular physical activity is one of the most effective ways to reduce the risk of heart disease, particularly for those with a family history. By engaging in regular exercise, you can help control weight, improve circulation, and lower cholesterol and blood pressure, all of which contribute to a healthier heart. Staying active is key to preventing heart disease family history, as it directly combats many of the risk factors associated with heart disease.

Exercise not only strengthens the heart muscle but also improves the function of the entire cardiovascular system. When you exercise, your heart pumps blood more efficiently, which helps to prevent plaque buildup in the arteries. In addition, regular exercise helps reduce stress and improve mental health, both of which are critical in managing overall heart health.
Best Types of Exercises for Heart Health
There are various types of exercises that are beneficial for heart health. Cardiovascular exercises such as walking, swimming, and cycling are particularly effective in improving heart function. These exercises increase the heart rate, boost circulation, and help the heart become more efficient at pumping blood throughout the body.
In addition to cardio, strength training is also important. Building muscle can help improve your body’s metabolism, reduce body fat, and maintain a healthy weight, all of which are important for reducing heart disease risk. Activities like weight lifting or resistance band exercises, when done regularly, can have long-term heart health benefits.
Lastly, flexibility exercises such as yoga or stretching can help maintain overall fitness and relieve stress. Stress management is crucial when working to prevent heart disease family history, and these exercises offer a low-impact way to stay active while improving mental well-being.
How Much Exercise Is Enough?
To effectively reduce the risk of heart disease, it’s recommended to aim for at least 150 minutes of moderate-intensity exercise each week. This can be broken down into 30 minutes of activity, five days a week. Activities like brisk walking, cycling, or swimming are ideal for meeting this goal.
For those who prefer more intense exercise, 75 minutes of vigorous activity, such as running or aerobics, can provide similar heart health benefits. It’s important to find an exercise routine that fits your lifestyle and is enjoyable, as this increases the likelihood of maintaining a consistent regimen over time.
In addition to the overall duration, incorporating both cardio and strength training into your routine ensures that you’re targeting multiple aspects of heart health. This combination can help improve heart function, lower blood pressure, and manage weight—all key elements in preventing heart disease family history.
Regular Medical Check-ups: Why They Are Crucial
When heart disease runs in your family, regular medical check-ups become crucial. These check-ups allow for early detection of any heart-related issues and help in managing risk factors before they escalate into serious problems. The earlier a potential problem is identified, the more options you have for treatment and prevention, making it easier to prevent heart disease family history.
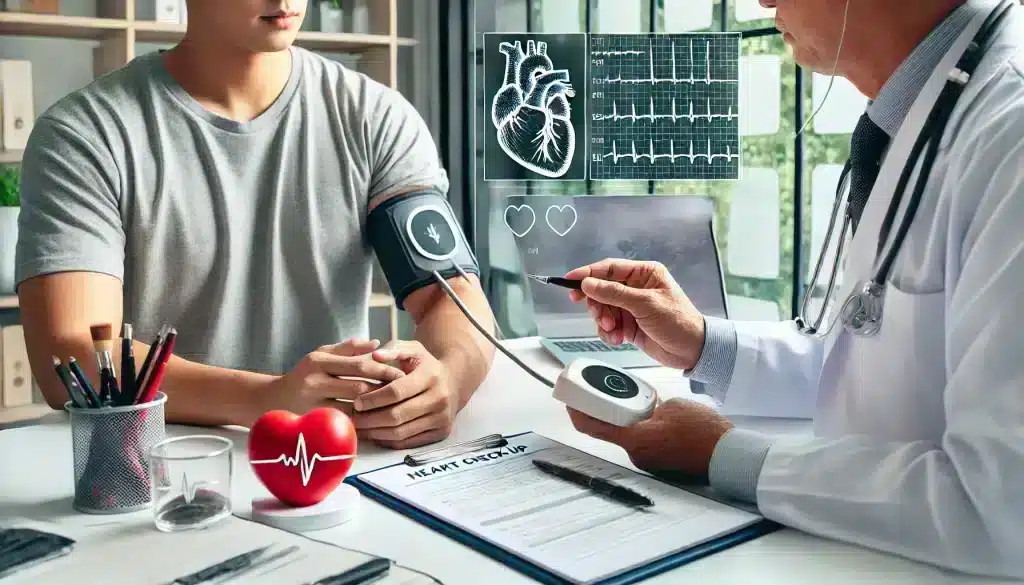
Doctors can track your heart health over time by performing routine tests such as blood pressure monitoring, cholesterol screenings, and electrocardiograms (ECG). These tests offer vital insights into how your heart is functioning and highlight areas where intervention might be necessary. If your family history includes early heart disease or heart attacks, staying vigilant with medical check-ups is key to managing your own risk.
Key Heart Health Tests You Should Take
Your healthcare provider will likely recommend several key tests to assess your heart health. Cholesterol screening measures your levels of low-density lipoprotein (LDL) and high-density lipoprotein (HDL), commonly referred to as “bad” and “good” cholesterol, respectively. High levels of LDL cholesterol can lead to plaque buildup in the arteries, increasing your risk of a heart attack or stroke.
Another common test is blood pressure monitoring, which is important because high blood pressure often has no symptoms but can cause serious damage to your heart and arteries over time. Additionally, an electrocardiogram (ECG) can detect irregularities in your heart’s rhythm that could point to underlying conditions, such as arrhythmias, that increase the risk of heart disease.
For those at higher risk, your doctor may suggest an echocardiogram, which uses ultrasound to take images of your heart, or a stress test, where your heart is monitored during physical activity to see how well it responds under stress. These tests can provide more detailed information about your heart’s health and its ability to handle exertion.
Monitoring Your Heart Health Over Time
Keeping track of your heart health should be an ongoing process, especially if you have a family history of heart disease. Regular check-ups, alongside lifestyle adjustments, help ensure that any emerging issues are addressed before they develop into more serious conditions. Even if you feel healthy, silent risk factors like high cholesterol or hypertension can exist, making frequent monitoring essential.
By having regular medical visits, you can work with your healthcare provider to create a personalized plan that fits your specific needs and genetic risk factors. This plan might include diet changes, exercise recommendations, and potentially medications aimed at preventing heart disease family history. Early detection and consistent monitoring are crucial components in maintaining long-term heart health.
Managing Stress and Its Impact on Heart Health
Chronic stress is a well-known contributor to heart disease, especially for individuals who have a family history of the condition. When stress levels remain elevated for extended periods, the body releases hormones like cortisol and adrenaline. While these hormones are helpful in short-term situations, prolonged exposure can cause inflammation, increase blood pressure, and strain the cardiovascular system, leading to heart disease. Managing stress effectively is critical in preventing heart disease family history.

Stress doesn’t just affect the heart directly. It also influences other behaviors that can increase heart disease risk. For example, people under stress might turn to unhealthy habits like overeating, smoking, or avoiding exercise, which further elevates the risk of heart problems. Being mindful of stress and developing strategies to manage it can have a profound impact on your overall heart health.
The Science Behind Stress and Heart Disease
When you’re stressed, your body’s natural fight-or-flight response kicks in. This leads to an increase in heart rate, higher blood pressure, and a release of stress hormones like cortisol. Over time, these reactions can cause damage to the blood vessels, increase the risk of blood clots, and ultimately lead to conditions like high blood pressure or heart attacks.
Research shows that stress also plays a role in the development of atherosclerosis, where the arteries become hardened and narrowed due to plaque buildup. Prolonged stress makes this process worse, increasing the likelihood of heart attacks or strokes. Stress management is key to preventing the negative physical effects on the heart.
Additionally, stress can exacerbate pre-existing conditions such as high cholesterol or hypertension, further increasing the risks. It’s essential to find effective ways to handle stress to avoid these long-term consequences, especially when there is a family history of heart disease.
Effective Stress Management Techniques
Several techniques can be highly effective in managing stress, helping to lower the risk of heart disease. Mindfulness and meditation are two proven methods that promote relaxation and reduce cortisol levels. Mindfulness practices help individuals focus on the present moment, which can reduce the mental clutter that often leads to stress.
Physical exercise is another powerful stress-relief tool. Engaging in regular physical activity, even for short durations, can improve mood and reduce stress. Exercise stimulates the production of endorphins, natural mood boosters, which can counteract the negative effects of stress.
Other methods like deep breathing exercises, progressive muscle relaxation, and hobbies such as reading or gardening can also provide stress relief. Finding what works best for you is important, and incorporating these techniques into your daily routine can make a significant difference in managing stress levels.
Medical Interventions and Treatments for Those at Risk
For individuals with a family history of heart disease, medical interventions may sometimes be necessary to manage risk factors and prevent the onset of heart disease. While lifestyle changes are the first line of defense, there are cases where medication or surgical interventions play a crucial role in preventing heart disease family history. These interventions can address specific risk factors like high cholesterol, hypertension, or blockages in the arteries, offering a proactive way to manage heart health.
Medical treatments are not a replacement for healthy living, but they can significantly enhance prevention efforts, especially when genetic predispositions make lifestyle changes alone insufficient. It’s important to work closely with your healthcare provider to identify the best approach for your specific risk factors and genetic background.
Medications for Heart Disease Prevention
There are several medications that doctors may prescribe to help lower the risk of heart disease in people with a family history of the condition. Statins are one of the most common medications used to lower LDL (“bad”) cholesterol levels, which can prevent plaque buildup in the arteries. These drugs are particularly effective for individuals with conditions like familial hypercholesterolemia.
In addition to statins, beta-blockers and ACE inhibitors are often used to manage high blood pressure, reducing the strain on the heart and preventing complications like heart attacks or strokes. These medications help control blood pressure by relaxing blood vessels, allowing for better blood flow and lowering the heart’s workload.
For those at high risk of blood clots, anticoagulants (blood thinners) may be prescribed. These drugs reduce the likelihood of clot formation, which can block arteries and lead to heart attacks. Working with a doctor to find the right medication, along with regular monitoring, ensures that these interventions are both safe and effective for preventing heart disease.
When Should Surgery Be Considered?
In some cases, surgical interventions may be necessary to address advanced heart disease or significant blockages in the arteries. One of the most common procedures is angioplasty, where a small balloon is inserted into a blocked artery to open it up and improve blood flow. A stent (a small mesh tube) is often placed in the artery to keep it open after the procedure.
For more severe cases, coronary artery bypass grafting (CABG) may be required. This surgery involves taking a healthy blood vessel from another part of the body and using it to bypass a blocked artery. Bypass surgery is typically reserved for individuals with multiple blocked arteries or those who have not responded well to other treatments.
Surgical interventions are often seen as a last resort but can be lifesaving for those with advanced heart disease. However, even after surgery, maintaining a healthy lifestyle and following medical advice are essential to prevent further complications.
Family Support and Education: Building a Strong Support System
When dealing with a family history of heart disease, building a strong support system is crucial. Family members can be an essential source of motivation, encouragement, and accountability. Engaging the family in discussions about heart disease, lifestyle changes, and risk management can create a healthier environment for everyone. A support system also helps reinforce heart-healthy behaviors, making it easier to prevent heart disease family history.
Education is a key component of this process. By ensuring that family members understand the risks, signs, and preventive measures related to heart disease, everyone can contribute to healthier choices. This collective effort not only improves individual health outcomes but also strengthens the bond between family members as they work together to lower the overall risk of heart disease.
Educating Family Members About Heart Disease
One of the first steps in building a supportive family network is to educate your loved ones about heart disease. Discussing the role that genetics play, along with the importance of lifestyle changes, helps everyone understand their own risk factors. Knowledge empowers people to make informed decisions about their health.
Family members should be aware of common risk factors such as high cholesterol, high blood pressure, and smoking. Encourage open conversations about how these factors affect heart health and what changes can be made. For example, reducing salt intake, quitting smoking, or becoming more physically active are steps everyone can take together to lower heart disease risk.
Additionally, educating children and younger family members about heart disease prevention from an early age instills heart-healthy habits for life. By setting a positive example, parents and older family members can guide the younger generation toward healthier lifestyles.
How Family Can Encourage Healthy Habits
Family involvement is key to adopting and maintaining heart-healthy habits. Meal planning and cooking together can make it easier to follow a heart-healthy diet. Opting for whole foods, reducing processed items, and focusing on nutrient-rich meals are steps that everyone in the household can take.
Similarly, exercising as a family can help make physical activity more enjoyable. Whether it’s taking a walk after dinner or scheduling family hikes on the weekend, being active together strengthens bonds while promoting heart health. Making exercise a regular part of the family routine increases the chances that everyone will stick with it.
In addition to diet and exercise, families can remind one another to attend regular medical check-ups and monitor heart health. Having a family member accompany you to doctor appointments or help track your progress can be incredibly motivating. A collective effort can make heart disease prevention more achievable for everyone involved.
Making Long-Term Changes for Heart Disease Prevention
Preventing heart disease, especially when there’s a family history involved, requires long-term commitment. It’s not just about making short-term adjustments but embracing sustainable lifestyle changes that can last a lifetime. These changes don’t have to happen overnight, but building healthy habits gradually is the key to preventing heart disease family history. Over time, these habits become part of your daily routine and significantly reduce your risk of developing heart-related issues.

One of the most important aspects of making long-term changes is setting realistic and achievable goals. Whether it’s improving your diet, increasing physical activity, or managing stress better, starting small ensures you don’t get overwhelmed. By creating an action plan that outlines specific steps, you set yourself up for success in the long term.
Setting Realistic Goals for Heart Health
Setting realistic goals is an essential part of any heart disease prevention plan. Instead of aiming for drastic changes, focus on small, measurable improvements. For instance, if your goal is to eat healthier, start by adding more vegetables to your meals rather than eliminating entire food groups all at once. Gradual changes are easier to maintain and more likely to lead to long-term success.
Similarly, with exercise, set achievable targets. If you’re not used to exercising regularly, try starting with short 10- to 15-minute walks, gradually building up to 30 minutes a day. Over time, you can increase the intensity and duration of your workouts as your fitness level improves. This step-by-step approach makes it easier to stick to your goals and avoid burnout.
Tracking your progress can also help keep you motivated. Whether it’s through journaling, using a fitness tracker, or simply marking your calendar, monitoring your improvements over time gives you a sense of accomplishment and helps you stay on track.
Tracking Progress and Staying Motivated
Consistency is crucial in maintaining long-term lifestyle changes. Tracking your progress is one of the most effective ways to ensure that you stay motivated over time. Whether it’s monitoring your cholesterol levels, tracking your daily steps, or recording the number of servings of fruits and vegetables you eat each day, keeping an eye on your progress allows you to make necessary adjustments along the way.
It’s also important to celebrate small victories. Every time you reach a milestone, such as lowering your blood pressure or sticking to an exercise routine for a month, take a moment to acknowledge your success. These small wins add up and reinforce your commitment to preventing heart disease in the long term.
Staying motivated can be challenging, especially during times of stress or when progress seems slow. Having a support system, whether it’s family, friends, or a healthcare provider, can make all the difference. Regularly reviewing your goals and staying flexible with your approach ensures that even if setbacks occur, you remain committed to improving your heart health over the long haul.
Case Studies: Real-Life Examples of Prevention Success
Real-life examples can offer valuable insights and inspiration for those looking to prevent heart disease family history. While everyone’s journey is unique, case studies of individuals who successfully managed their heart disease risk can serve as a reminder that with the right steps, it’s possible to overcome genetic predispositions.

The following case studies highlight how proactive measures, from lifestyle changes to medical interventions, helped these individuals manage their heart health despite a strong family history of heart disease. Their stories illustrate the power of early detection, consistency, and support from healthcare providers and family members.
Case Study 1: Overcoming Family History of Heart Disease Through Lifestyle Changes
John, a 50-year-old man, comes from a family where heart disease has been common. His father and grandfather both had heart attacks before the age of 60. Concerned about his genetic risk, John decided to take proactive steps in his 30s to improve his heart health.
John started by focusing on his diet. He reduced his intake of saturated fats and began eating more fruits, vegetables, and whole grains. He also incorporated regular physical activity into his routine, starting with brisk walks and eventually working his way up to jogging and strength training. Over the years, John consistently attended medical check-ups, monitored his cholesterol levels, and maintained a healthy weight.
Now at 50, John has not only avoided heart disease but has also encouraged his family members to adopt similar habits. His story is a testament to how making sustainable lifestyle changes can significantly reduce the risk of heart disease, even when it runs in the family.
Case Study 2: Combining Lifestyle Changes and Medical Intervention
Sarah, 45, had a family history of heart attacks, with her father suffering from one at age 55 and her older brother experiencing chest pains by age 50. Aware of her genetic risk, Sarah adopted heart-healthy habits early on, but her cholesterol levels remained high despite her efforts.
After discussing her options with her doctor, Sarah was prescribed statins to help lower her cholesterol. This medication, combined with her commitment to a heart-healthy diet and regular exercise, significantly improved her heart health. Sarah’s case shows how medical interventions can complement lifestyle changes to provide comprehensive heart disease prevention.
By being proactive and working closely with her healthcare provider, Sarah has managed to avoid the heart problems that affected her father and brother. Her success highlights the importance of early intervention and the combination of lifestyle adjustments and medical treatment when necessary.
Frequently Asked Questions
1. Can heart disease be prevented if it runs in my family?
Yes, even if you have a family history of heart disease, you can take steps to reduce your risk. Adopting a heart-healthy lifestyle, managing stress, and attending regular medical check-ups are all important measures in preventing heart disease.
2. What role does diet play in preventing heart disease?
Diet plays a crucial role in heart disease prevention. A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can reduce cholesterol, control blood pressure, and maintain a healthy weight, all of which lower the risk of heart disease.
3. How often should I get my cholesterol and blood pressure checked?
For those with a family history of heart disease, it is recommended to have your cholesterol and blood pressure checked at least once a year. Your doctor may advise more frequent monitoring depending on your risk factors.
4. What types of exercises are best for heart health?
Cardiovascular exercises such as walking, swimming, and cycling are excellent for heart health. Strength training and flexibility exercises like yoga can also support overall cardiovascular health.
5. How does stress contribute to heart disease?
Chronic stress causes the release of hormones like cortisol, which can raise blood pressure and cause inflammation. Over time, this can lead to heart disease by damaging the arteries and increasing the risk of heart attacks.
6. Can medications help prevent heart disease?
Yes, medications like statins, beta-blockers, and ACE inhibitors are often prescribed to help manage cholesterol, blood pressure, and other risk factors in individuals with a family history of heart disease.
7. Is heart disease hereditary?
Yes, certain genetic factors can increase your risk of developing heart disease. However, lifestyle changes and medical interventions can help mitigate these risks, even if heart disease runs in your family.
8. How can I reduce my cholesterol levels naturally?
To lower cholesterol naturally, focus on eating a diet high in fiber and healthy fats like omega-3s, reduce your intake of saturated and trans fats, and engage in regular physical activity. Avoiding smoking and managing stress are also helpful.
9. What should I ask my doctor if heart disease runs in my family?
Ask about your specific risk factors, recommended screenings, and lifestyle changes you can make to reduce your risk. It’s also important to discuss whether you might benefit from medications or genetic testing.
10. Can young people develop heart disease if it runs in their family?
Yes, young people can develop heart disease, particularly if there is a strong family history or if they have other risk factors like high cholesterol or high blood pressure. Early prevention is key in reducing these risks.
11. What is the role of genetic testing in heart disease prevention?
Genetic testing can identify specific inherited conditions that increase the risk of heart disease, such as familial hypercholesterolemia. Knowing your genetic predisposition can help guide preventive strategies.
12. How does smoking affect heart disease risk?
Smoking is a major risk factor for heart disease. It damages the arteries, raises blood pressure, and reduces oxygen in the blood, increasing the likelihood of heart attacks, especially in individuals with a family history of heart disease.
13. What are the signs that I might be at risk for heart disease?
Common signs include high blood pressure, high cholesterol, obesity, and a family history of heart disease. If you experience chest pain, shortness of breath, or irregular heartbeats, you should see a doctor immediately.
14. Can heart disease be reversed once diagnosed?
While heart disease cannot always be fully reversed, it can be managed effectively with lifestyle changes and medical treatments. Catching it early through regular check-ups makes it easier to prevent further damage.
15. How can family members support someone at risk of heart disease?
Family members can support by encouraging heart-healthy habits, such as cooking nutritious meals, exercising together, and reminding one another to attend regular medical check-ups.