Understanding Heart Disease: A Brief Overview
Heart disease, also known as cardiovascular disease, encompasses a range of conditions affecting the heart’s structure and function. It remains one of the leading causes of death worldwide, contributing significantly to morbidity and healthcare costs. Common types of heart disease include coronary artery disease, heart failure, arrhythmias, and valvular heart disease. These conditions are often driven by a combination of lifestyle factors, genetic predisposition, and other health conditions such as hypertension, diabetes, and high cholesterol.
Traditionally, heart disease has been managed through lifestyle modifications, medications, and surgical interventions. However, advancements in medical research and technology are paving the way for more effective and personalized treatments, offering hope for improved outcomes and quality of life for patients. Understanding the latest innovations in heart disease treatments is crucial for healthcare professionals, patients, and anyone interested in the evolving landscape of cardiology.
Traditional Treatments for Heart Disease
Traditional treatments for heart disease have focused on managing symptoms, preventing progression, and reducing the risk of complications. These approaches typically include lifestyle changes, such as adopting a heart-healthy diet, regular exercise, smoking cessation, and stress management. Medications also play a crucial role in treatment, with commonly used drugs including statins, beta-blockers, ACE inhibitors, and antiplatelet agents, each targeting different aspects of heart disease.
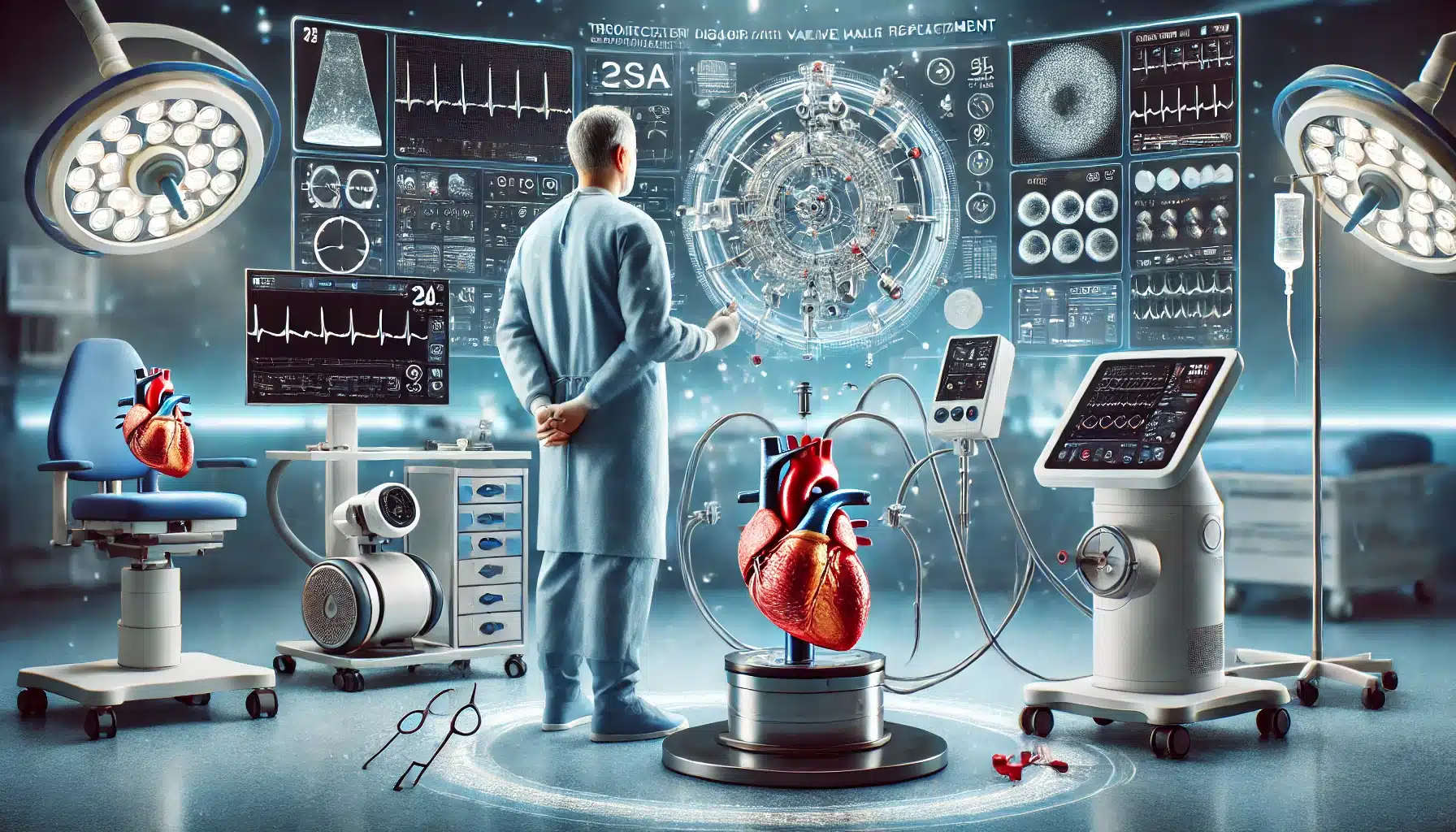
Surgical interventions have been a cornerstone of heart disease treatment, especially for advanced cases. Procedures such as coronary artery bypass grafting (CABG), angioplasty with stent placement, and valve replacement or repair have proven effective in restoring blood flow, correcting structural abnormalities, and improving heart function. Despite the effectiveness of these traditional treatments, there is a growing need for less invasive and more personalized approaches, which has led to significant innovations in the field.
Emerging Technologies in Heart Disease Treatment
Recent advancements in medical technology have introduced a range of minimally invasive procedures that offer alternatives to traditional surgery. These innovations aim to reduce recovery times, minimize complications, and improve patient outcomes. One such approach is transcatheter aortic valve replacement (TAVR), a procedure that allows for the replacement of a diseased aortic valve without open-heart surgery. This technique is particularly beneficial for patients who are considered high-risk for conventional surgery.
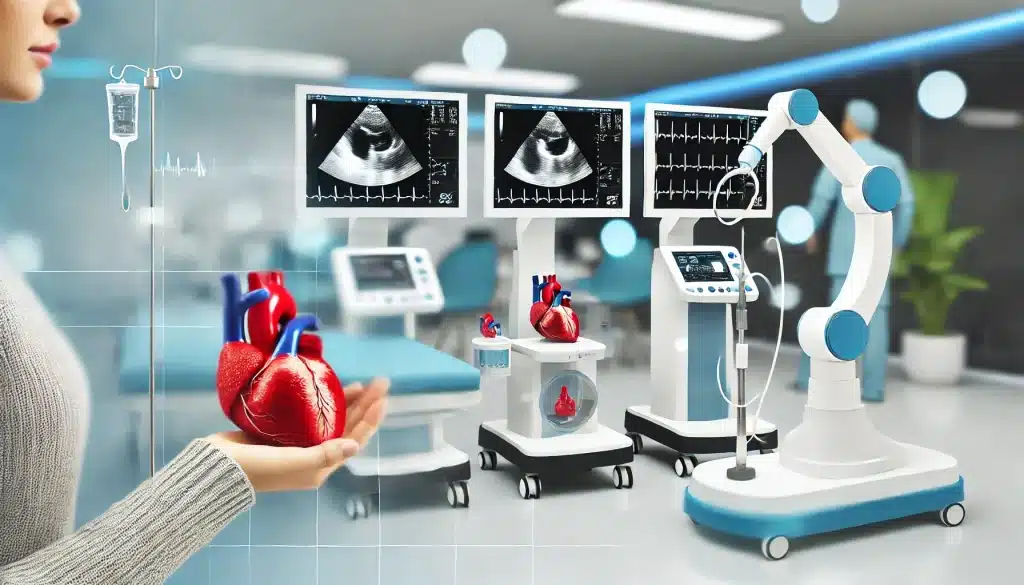
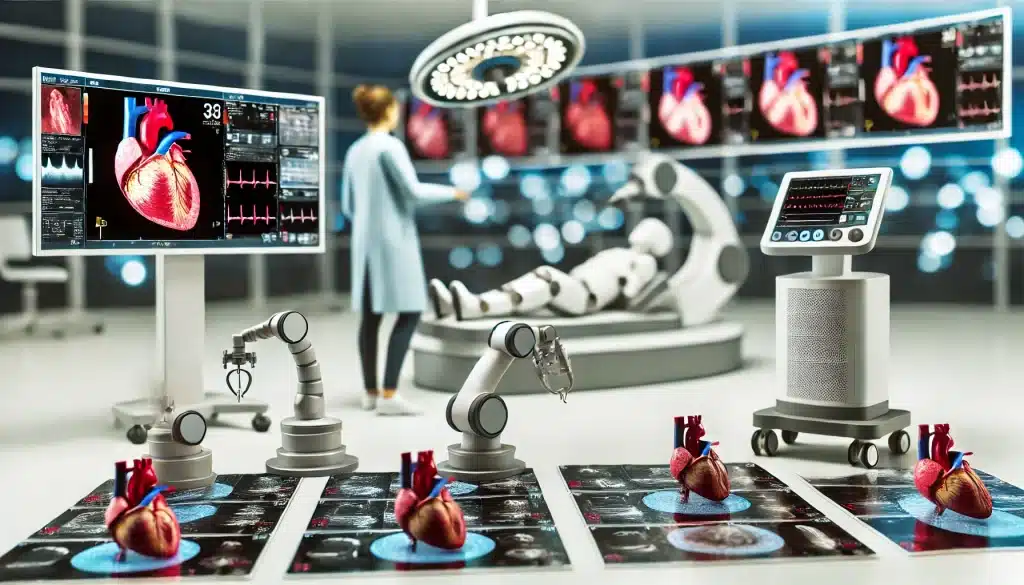
Another notable advancement is the use of advanced imaging technologies, such as 3D echocardiography and cardiac MRI, which provide detailed insights into the heart’s structure and function. These tools enable more precise diagnosis and treatment planning, helping to tailor interventions to the specific needs of each patient. The integration of robotics in surgical procedures has also revolutionized heart disease treatment, allowing for greater precision and control during operations.
Minimally Invasive Procedures
Minimally invasive procedures are transforming the landscape of heart disease treatment by offering safer alternatives to traditional surgeries. Techniques such as percutaneous coronary intervention (PCI), also known as coronary angioplasty, use a catheter to open blocked arteries, improving blood flow to the heart. This approach reduces the need for large incisions and extensive recovery times, making it an attractive option for many patients.
Another emerging procedure is the mitral clip, used to treat mitral regurgitation by clipping together the leaflets of the mitral valve, thereby reducing backflow and improving heart efficiency. These minimally invasive options not only lower the risk of complications but also provide faster recovery and improved quality of life for patients.
Advanced Drug Therapies
Advances in pharmacology have led to the development of new drug therapies that target specific pathways involved in heart disease. One example is PCSK9 inhibitors, a class of drugs that significantly lower LDL cholesterol levels, reducing the risk of heart attacks and strokes. Additionally, novel anticoagulants, such as direct oral anticoagulants (DOACs), offer safer and more convenient alternatives to traditional blood thinners like warfarin, with fewer dietary restrictions and monitoring requirements.
Another promising area of drug development is in the use of SGLT2 inhibitors, initially designed for diabetes management but now recognized for their cardiovascular benefits, including heart failure risk reduction. These advanced drug therapies represent a major step forward in the medical management of heart disease, providing more targeted and effective treatment options for patients.
The Role of Genetics and Personalized Medicine
The advent of personalized medicine has revolutionized the approach to treating heart disease by tailoring interventions based on an individual’s genetic profile, lifestyle, and specific health needs. Genetics play a significant role in heart disease, influencing factors such as cholesterol levels, blood pressure, and the risk of developing conditions like cardiomyopathy or arrhythmias. With advancements in genetic testing, it is now possible to identify individuals at higher risk of heart disease even before symptoms appear, enabling earlier and more targeted interventions.
Personalized medicine also extends to the development of individualized treatment plans that consider a patient’s unique genetic makeup. This approach can help determine the most effective medications, dosages, and lifestyle modifications, ultimately leading to better outcomes and fewer side effects. For instance, pharmacogenomics—the study of how genes affect a person’s response to drugs—allows healthcare providers to select medications that are most likely to be effective for a particular patient, reducing the trial-and-error aspect of treatment.
Genetic Testing and Risk Assessment
Genetic testing is becoming an increasingly valuable tool in assessing heart disease risk. Tests such as whole genome sequencing and targeted gene panels can identify genetic mutations associated with conditions like familial hypercholesterolemia, hypertrophic cardiomyopathy, and other inherited cardiac disorders. By understanding a patient’s genetic risk factors, healthcare providers can recommend preventive measures or early interventions that may significantly alter the course of the disease.
In addition to identifying risk, genetic testing can also guide treatment decisions. For example, patients with specific genetic variations may respond better to certain medications or may be at higher risk for adverse reactions, allowing for more personalized and safer treatment choices. As genetic testing becomes more accessible and affordable, it is expected to play a central role in the future of heart disease management.
Tailored Treatment Plans
Tailored treatment plans take into account not only a patient’s genetic information but also other factors such as age, gender, lifestyle, and comorbidities. This holistic approach allows for more precise and effective management of heart disease. For example, patients with specific genetic profiles may benefit more from particular types of exercise or dietary adjustments, enhancing the overall effectiveness of lifestyle interventions.
Additionally, tailored treatment plans can optimize medication regimens. For example, in patients with certain genetic markers that affect how their body metabolizes drugs, personalized dosing strategies can help achieve therapeutic benefits while minimizing the risk of side effects. This level of customization in heart disease treatment represents a significant advancement in the effort to provide care that is as unique as the patient themselves.
Cutting-Edge Medical Devices
Innovations in medical devices are playing a critical role in the treatment and management of heart disease. From implantable devices that help regulate heart function to wearable technology that provides continuous monitoring, these advancements are helping to improve patient outcomes and quality of life. Implantable devices, such as pacemakers and defibrillators, have been around for decades, but recent innovations have made them smaller, more efficient, and capable of more complex functions.
For instance, newer pacemakers are equipped with remote monitoring capabilities, allowing healthcare providers to track a patient’s heart rhythm and make necessary adjustments without the need for frequent office visits. Implantable cardioverter-defibrillators (ICDs) not only monitor heart rhythms but can also deliver life-saving shocks in the event of a severe arrhythmia, providing peace of mind for patients with high risk of sudden cardiac arrest.
Implantable Devices
Implantable devices have evolved significantly, offering new solutions for patients with heart disease. One example is the development of leadless pacemakers, which are much smaller than traditional pacemakers and do not require leads (wires) that connect the device to the heart. This reduces the risk of complications such as lead displacement or infection, making them a safer alternative for certain patients.
Another cutting-edge device is the left ventricular assist device (LVAD), which helps pump blood from the left ventricle to the rest of the body in patients with severe heart failure. LVADs are often used as a bridge to heart transplantation or as a long-term therapy for patients who are not candidates for transplant. As these devices continue to improve, they offer hope for better management of advanced heart disease.
Wearable Technology for Heart Monitoring
Wearable technology is increasingly being used to monitor heart health and detect early signs of heart disease. Devices such as smartwatches equipped with ECG capabilities can detect irregular heart rhythms, such as atrial fibrillation, and alert users to seek medical attention. This real-time monitoring allows for earlier detection and intervention, potentially preventing more serious complications.
In addition to ECG monitoring, wearable devices can track other vital signs such as heart rate, blood pressure, and oxygen saturation, providing a comprehensive view of a patient’s cardiovascular health. The data collected by these devices can be shared with healthcare providers, enabling more proactive and personalized care. As wearable technology continues to advance, it holds the promise of transforming how we monitor and manage heart disease on a day-to-day basis.
The Impact of Artificial Intelligence in Cardiology
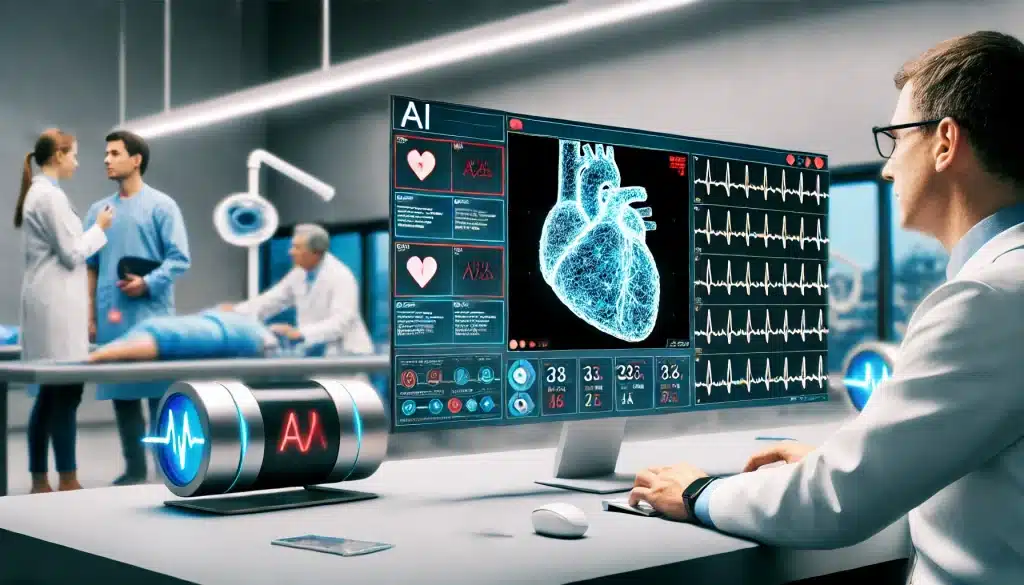
Artificial Intelligence (AI) is making significant strides in the field of cardiology, providing tools that enhance diagnosis, treatment planning, and patient management. AI algorithms can analyze vast amounts of data from medical records, imaging studies, and genetic information to identify patterns that may be missed by human analysis. This capability is particularly valuable in diagnosing complex conditions, predicting patient outcomes, and optimizing treatment plans based on individualized data.
One of the most promising applications of AI in cardiology is in predictive analytics, where AI models can forecast the likelihood of events such as heart attacks or strokes based on a patient’s health data. This proactive approach allows for earlier interventions and personalized risk reduction strategies. AI is also being used to improve the accuracy of diagnostic tools, such as echocardiograms and CT scans, by providing more precise measurements and identifying subtle abnormalities that might be overlooked.
AI in Diagnosis
AI is transforming the diagnostic process in cardiology by enhancing the accuracy and speed of interpreting complex medical images. Machine learning algorithms, a subset of AI, can be trained to recognize specific patterns associated with various heart conditions. For example, AI can assist in analyzing echocardiograms to detect heart valve abnormalities, ventricular dysfunction, or other structural issues with high accuracy.
Additionally, AI-powered software can assist radiologists and cardiologists by automating the analysis of cardiac MRI and CT scans, reducing the time required for diagnosis and minimizing the potential for human error. This technology not only improves diagnostic precision but also makes advanced imaging techniques more accessible in clinical practice, ultimately leading to better patient outcomes.
AI in Treatment Planning
AI’s role extends beyond diagnosis, playing a crucial part in treatment planning and decision-making. Predictive models can help determine the most effective treatment strategies for individual patients, considering factors such as disease severity, comorbidities, and potential response to various therapies. For instance, AI can assist in identifying patients who would benefit most from specific interventions, such as coronary artery bypass surgery versus percutaneous coronary intervention.
Moreover, AI is being used to develop personalized medication regimens. By analyzing a patient’s genetic information and health data, AI can recommend optimal drug combinations and dosages, minimizing adverse effects and enhancing therapeutic efficacy. This level of personalized care represents a significant shift from the traditional one-size-fits-all approach to a more tailored and effective strategy in managing heart disease.

Future Prospects in Heart Disease Treatments
The future of heart disease treatment is likely to be shaped by continued advancements in technology, genetics, and personalized medicine. Researchers are exploring innovative therapies such as gene editing, which holds the potential to correct genetic defects that cause certain types of heart disease. Techniques like CRISPR-Cas9 are being investigated for their ability to modify genes associated with high cholesterol, heart failure, and other cardiovascular conditions, offering a new frontier in disease prevention and treatment.
Regenerative medicine, including the use of stem cells to repair damaged heart tissue, is another promising area of research. Scientists are working on ways to regenerate heart muscle and blood vessels, potentially reversing damage caused by heart attacks or chronic heart disease. These approaches, while still in the experimental stages, could revolutionize the way we treat heart disease, moving from managing symptoms to actually repairing the heart itself.
In addition to these biological innovations, the integration of digital health technologies, such as telemedicine and mobile health apps, is expected to play a growing role in heart disease management. These tools can provide patients with real-time access to healthcare providers, personalized health recommendations, and ongoing monitoring of heart health, making it easier to manage chronic conditions and maintain a heart-healthy lifestyle.
Conclusion: The Future of Heart Health Care
The landscape of heart disease treatment is rapidly evolving, driven by innovations in technology, genetics, and personalized medicine. From minimally invasive procedures and advanced drug therapies to cutting-edge medical devices and AI-powered tools, the future of cardiology promises more precise, effective, and patient-centered care. As these advancements continue to develop, they offer hope for better management of heart disease, improved patient outcomes, and ultimately, a reduction in the global burden of cardiovascular disease.
Staying informed about the latest innovations in heart disease treatments is essential for patients, healthcare providers, and researchers alike. By embracing these new technologies and approaches, we can move closer to a future where heart disease is not only treatable but preventable, enhancing the quality of life for millions of people worldwide.
What are the latest minimally invasive procedures for heart disease?
The latest minimally invasive procedures include transcatheter aortic valve replacement (TAVR), percutaneous coronary intervention (PCI), and mitral clip procedures, which reduce the need for open-heart surgery and offer quicker recovery times.
How is artificial intelligence used in heart disease treatment?
AI is used in cardiology to enhance the accuracy of diagnoses, predict patient outcomes, and develop personalized treatment plans. AI-powered tools analyze medical data to identify patterns and provide insights that improve patient care.
What role does genetics play in heart disease treatment?
Genetics helps identify individuals at risk for heart disease and allows for personalized treatment plans based on genetic profiles. Genetic testing can guide decisions on the most effective medications and interventions.
Are wearable devices effective for monitoring heart health?
Yes, wearable devices such as smartwatches with ECG capabilities can monitor heart rhythms, detect abnormalities like atrial fibrillation, and provide real-time data that helps manage heart health more effectively.
What future technologies are being developed for heart disease treatment?
Future technologies include gene editing, regenerative medicine with stem cells, and the continued integration of digital health tools like telemedicine and mobile health apps, which will further personalize and improve heart disease management.