Understanding Climate Change and Its Impact on Health
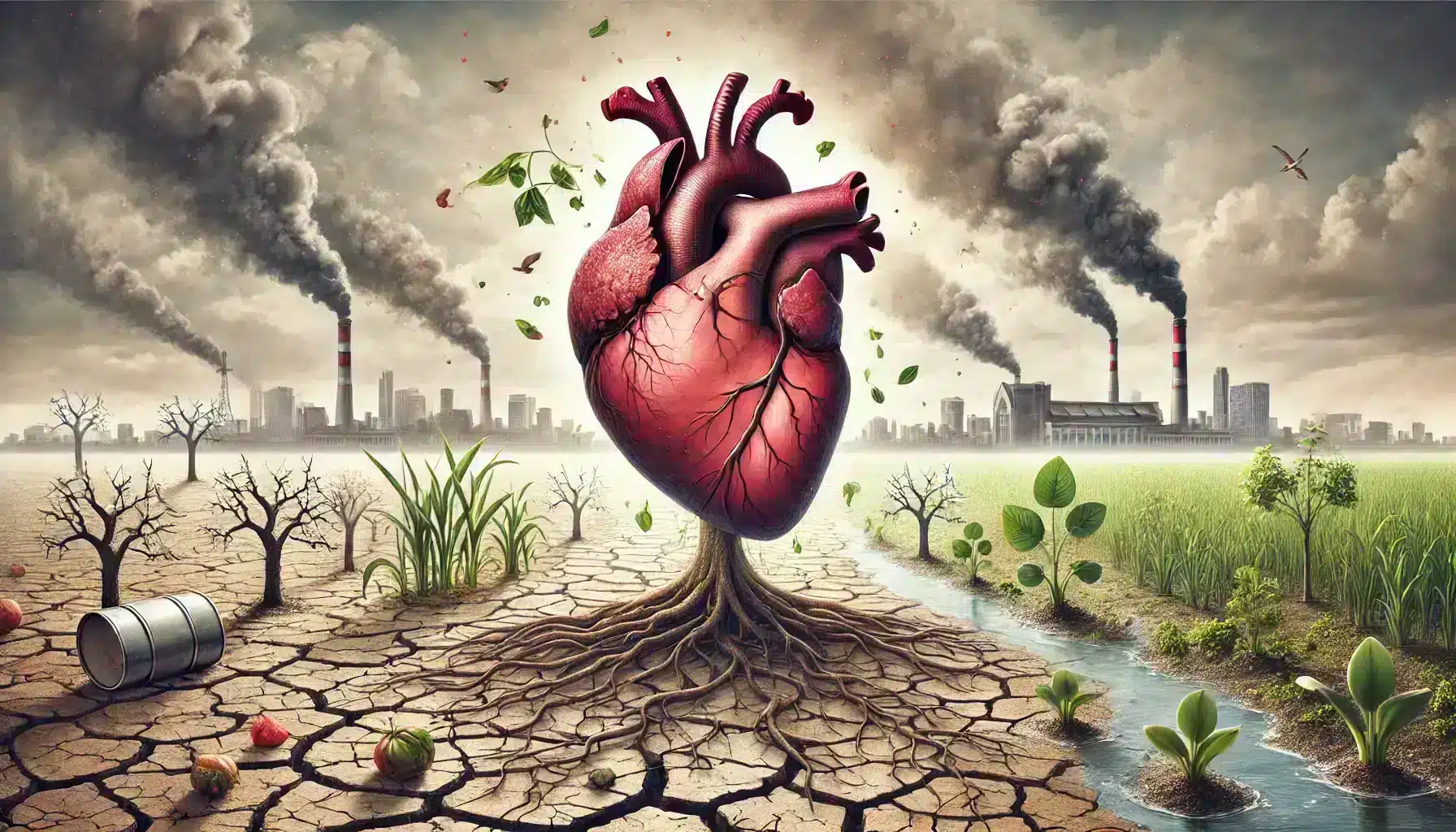
Climate change refers to long-term shifts in temperatures and weather patterns, primarily due to human activities such as burning fossil fuels, deforestation, and industrial processes. These activities increase the concentration of greenhouse gases like carbon dioxide and methane in the atmosphere, leading to global warming and other environmental changes.
While climate change is often associated with environmental impacts, it also poses significant threats to human health. The consequences of a changing climate, such as extreme weather events, rising temperatures, and increased air pollution, have far-reaching effects on various aspects of health, including cardiovascular health. Understanding these impacts is crucial to developing strategies to protect vulnerable populations and mitigate health risks.
Temperature Extremes and Cardiovascular Risks
Extreme temperatures, both hot and cold, can have adverse effects on cardiovascular health. Heatwaves, which are becoming more frequent and intense due to climate change, can lead to heat stress, dehydration, and an increased risk of heart attacks and strokes. High temperatures force the heart to work harder to cool the body, especially in individuals with existing heart conditions, elderly people, and those with limited access to air conditioning.
Cold weather, on the other hand, causes blood vessels to constrict, which increases blood pressure and can lead to heart attacks or strokes. As climate change disrupts normal weather patterns, the frequency and severity of these temperature extremes are expected to rise, posing ongoing risks to cardiovascular health.
The Connection Between Climate Change and Heart Health
Air Pollution and Its Effects on Cardiovascular System
Air pollution, a major byproduct of fossil fuel combustion and industrial activities, has been strongly linked to cardiovascular diseases. Particulate matter (PM), nitrogen oxides, sulfur dioxide, and ground-level ozone are some of the pollutants that contribute to poor air quality, which is exacerbated by climate change. These pollutants can enter the bloodstream through the lungs, causing inflammation, oxidative stress, and impaired blood vessel function, leading to an increased risk of heart attacks, strokes, and other cardiovascular conditions.
Research indicates that long-term exposure to high levels of air pollution can accelerate the progression of atherosclerosis, a condition where plaque builds up in the arteries, narrowing them and restricting blood flow. This not only affects individuals with pre-existing heart conditions but also increases the risk for those without prior health issues, making air quality management a critical component of cardiovascular health strategies in the context of climate change.
Impact of Natural Disasters and Stress on Heart Health
Climate change contributes to the increased frequency and intensity of natural disasters such as hurricanes, floods, wildfires, and droughts. These events can have immediate and long-term impacts on cardiovascular health. The physical stress from such disasters can trigger heart attacks, especially in individuals with pre-existing heart conditions. Additionally, the psychological stress associated with the loss of homes, displacement, and trauma can exacerbate cardiovascular problems by increasing blood pressure, heart rate, and stress hormone levels.
Post-disaster environments often involve disruptions in healthcare services, limited access to medications, and poor living conditions, further aggravating cardiovascular risks. It is essential to understand these connections to prepare and protect vulnerable populations from the compounded effects of climate change and natural disasters on heart health.

Vulnerable Populations: Who is Most at Risk?
Elderly and Chronic Disease Patients
The elderly and individuals with chronic health conditions, such as heart disease, hypertension, and diabetes, are among the most vulnerable populations when it comes to the cardiovascular impacts of climate change. As the body ages, its ability to regulate temperature diminishes, making older adults more susceptible to heat stress during extreme temperature events. Additionally, pre-existing conditions can be exacerbated by climate-induced factors like air pollution and stress from natural disasters, increasing the risk of adverse cardiovascular events.
Medications commonly used by elderly patients, such as diuretics and beta-blockers, can also affect the body’s ability to respond to heat, further compounding the risk. It is crucial to develop targeted interventions and healthcare strategies to protect these vulnerable groups from the escalating effects of climate change on cardiovascular health.
Low-Income Communities and Accessibility Issues
Low-income communities often face greater exposure to the negative effects of climate change and are less equipped to handle these impacts due to limited access to healthcare, safe housing, and resources for adaptation. These communities are more likely to live in areas with higher pollution levels, such as near highways or industrial zones, increasing their exposure to harmful pollutants that contribute to cardiovascular disease.
Furthermore, economic barriers can restrict access to healthcare, preventive services, and necessary medications, making it more challenging for individuals in these communities to manage their cardiovascular health. Efforts to address the health impacts of climate change must include policies and programs that focus on improving environmental conditions, healthcare access, and economic opportunities for low-income populations.
Prevention Strategies for Protecting Heart Health
Personal Lifestyle Changes
Individuals can take proactive steps to protect their cardiovascular health in the face of climate change. Adopting a heart-healthy lifestyle, which includes a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, can help mitigate the risks associated with environmental changes. Regular physical activity is also crucial, though it should be adapted to weather conditions—opting for indoor exercises during extreme temperatures or high pollution days can help reduce exposure to harmful elements.
Staying hydrated, managing stress through mindfulness practices, and avoiding tobacco use are additional measures that can support heart health. It is also essential for individuals to stay informed about air quality indices and weather advisories, allowing them to plan outdoor activities when conditions are safer. Personal preparedness, such as having a plan for extreme weather events, can further protect heart health by reducing stress and ensuring access to necessary medications during emergencies.
Community and Policy-Level Actions
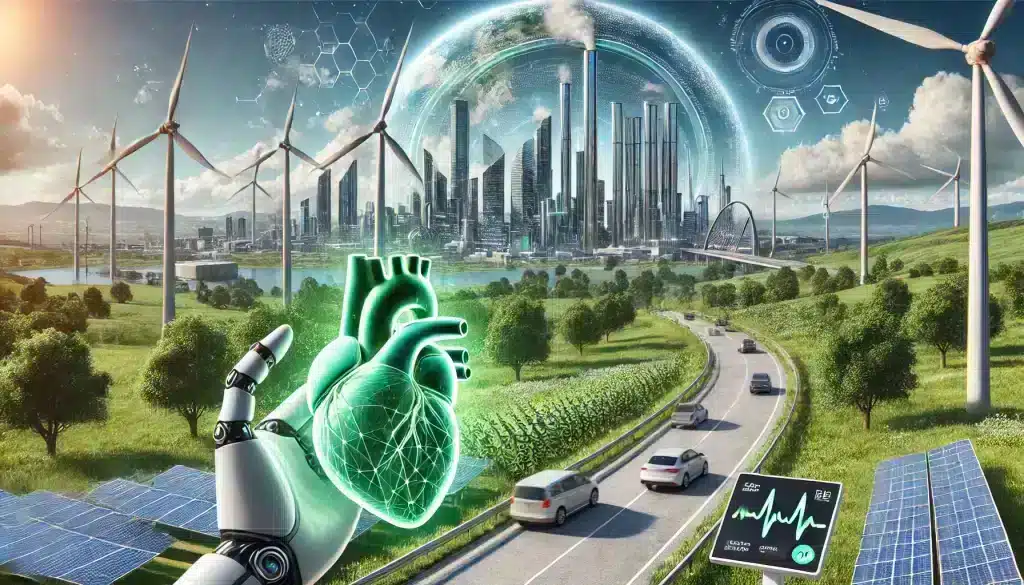
Addressing the cardiovascular impacts of climate change requires collective action at the community and policy levels. Local governments and organizations can implement measures to improve air quality, such as reducing emissions from vehicles and industries, promoting the use of public transportation, and increasing green spaces in urban areas. Policies that encourage the use of renewable energy sources and energy-efficient technologies can also help mitigate the effects of climate change on public health.
Public health campaigns that raise awareness about the connection between climate change and cardiovascular health can empower communities to take action. Additionally, healthcare systems need to prepare for the increased demand for cardiovascular care, particularly during extreme weather events and natural disasters. By integrating climate resilience into healthcare planning and infrastructure, communities can better protect their populations from the health impacts of a changing climate.
Future Implications: What Can Be Done?
Research and Technological Advances
Ongoing research is crucial to understanding the complex relationship between climate change and cardiovascular health. Advancements in technology and data analysis allow researchers to better predict the health impacts of climate-related factors, such as heatwaves and pollution, and to identify the most effective interventions. For instance, wearable devices and mobile health apps can monitor heart health in real-time, providing individuals with personalized insights and early warnings during extreme weather events.
Innovations in healthcare delivery, such as telemedicine, can also play a significant role in making cardiovascular care more accessible, especially during natural disasters or in remote areas. Investment in research that explores the development of new treatments and preventive measures, tailored to the challenges posed by climate change, will be vital in reducing the burden of cardiovascular diseases in the future.
Global and Local Initiatives
Tackling the cardiovascular impacts of climate change requires coordinated efforts at both global and local levels. International agreements, such as the Paris Agreement, aim to limit global warming by reducing greenhouse gas emissions, which in turn can mitigate the health impacts of climate change. Local governments and communities also play a key role by implementing policies that promote sustainability, improve air quality, and enhance public health infrastructure.
Programs that focus on climate adaptation, such as creating cooling centers during heatwaves or building flood-resistant infrastructure, can help protect vulnerable populations from extreme weather events. Community-based initiatives that engage residents in environmental conservation and climate action can foster resilience and reduce health disparities. By integrating health considerations into climate policies and emphasizing preventive care, we can work towards a future where the cardiovascular impacts of climate change are minimized.
Conclusion: Moving Forward in a Changing Climate
The relationship between climate change and cardiovascular health is complex and multifaceted, affecting individuals and communities in diverse ways. As we continue to experience the impacts of a changing climate, it is essential to prioritize both individual and collective actions to protect heart health. This includes making lifestyle changes, advocating for cleaner environments, and supporting policies that address the root causes of climate change.
By understanding the risks and taking proactive measures, we can reduce the cardiovascular burden of climate change and promote healthier, more resilient communities. The journey towards a sustainable future is not only about protecting the environment but also about safeguarding the health and well-being of all people.
Frequently Asked Questions (FAQ)
1. How does climate change directly affect cardiovascular health?
Climate change affects cardiovascular health through various mechanisms, including extreme temperatures, increased air pollution, and stress from natural disasters. These factors can lead to increased risks of heart attacks, strokes, and other cardiovascular conditions, particularly in vulnerable populations such as the elderly and those with pre-existing health conditions.
2. What are the main pollutants that impact heart health in the context of climate change?
Key pollutants that affect heart health include particulate matter (PM), nitrogen oxides, sulfur dioxide, and ground-level ozone. These pollutants are often byproducts of fossil fuel combustion and industrial activities and can exacerbate cardiovascular conditions by causing inflammation and oxidative stress in the body.
3. Who is most at risk of cardiovascular impacts due to climate change?
Vulnerable populations include the elderly, individuals with chronic diseases such as heart disease and diabetes, and low-income communities with limited access to healthcare and resources. These groups are more susceptible to the adverse effects of climate change, such as heat stress, air pollution, and disruptions caused by natural disasters.
4. What steps can individuals take to protect their heart health in a changing climate?
Individuals can protect their heart health by adopting a healthy lifestyle, staying informed about air quality and weather conditions, and being prepared for extreme weather events. This includes eating a balanced diet, exercising indoors during poor air quality days, managing stress, and avoiding tobacco use.
5. How can communities and governments help reduce the cardiovascular impacts of climate change?
Communities and governments can help by implementing policies that improve air quality, reduce greenhouse gas emissions, and enhance public health infrastructure. Public health campaigns, climate adaptation programs, and investments in renewable energy and sustainable practices are essential to reducing the cardiovascular impacts of climate change on populations.