Introduction to Heart Valve Disease
Overview of Heart Valve Disease
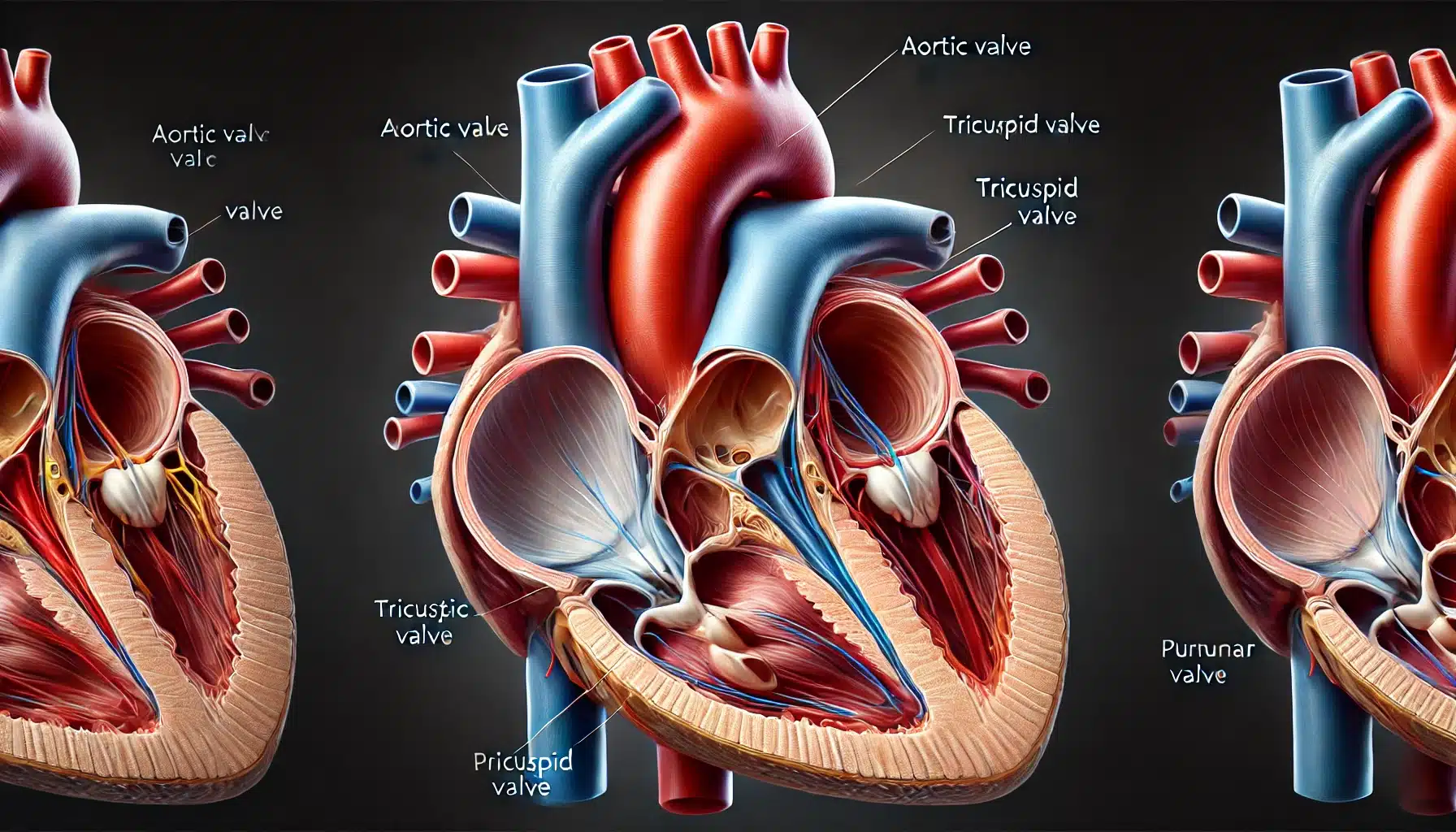
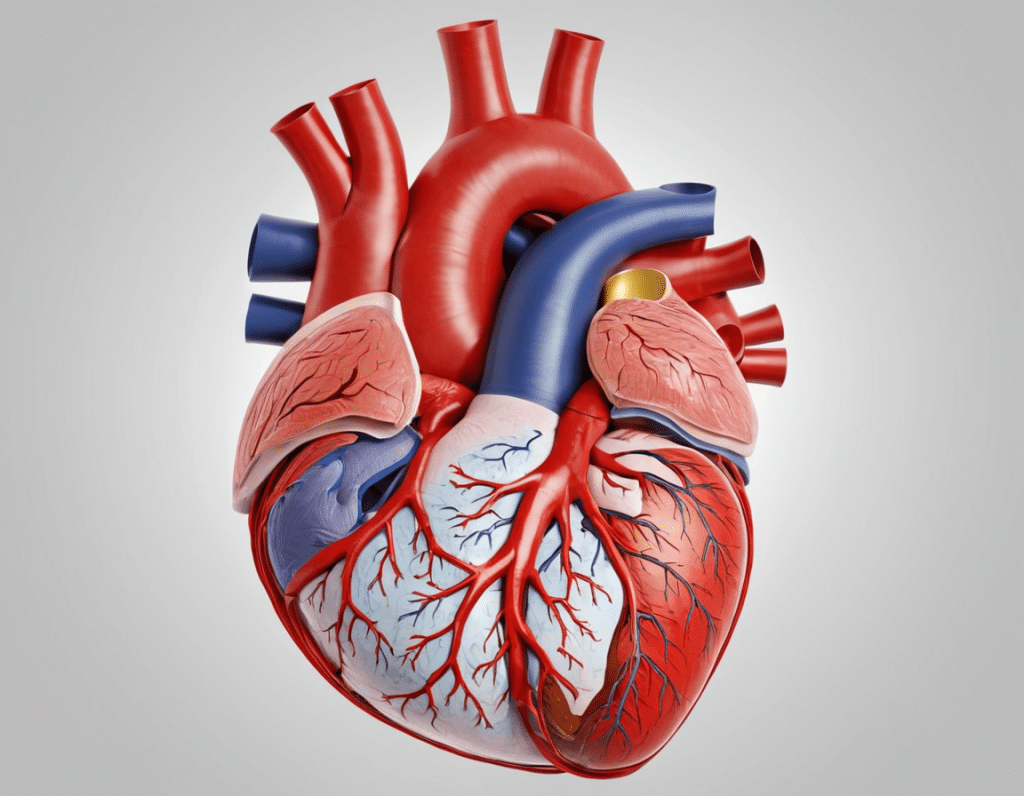
Heart valve disease is a condition that affects one or more of the heart’s four valves: the aortic, mitral, tricuspid, and pulmonary valves. These valves play a critical role in controlling the direction and flow of blood through the heart. They ensure that blood moves efficiently from one chamber to another and prevents backflow, which is essential for maintaining proper circulation throughout the body. When these valves do not function correctly, it can lead to heart valve disease, disrupting the normal flow of blood and putting additional strain on the heart.
There are two main types of heart valve problems: stenosis and regurgitation. Stenosis occurs when a valve does not open fully, causing a reduction in blood flow. Regurgitation, on the other hand, happens when a valve does not close properly, allowing blood to leak backward. Both conditions can lead to serious health complications if not treated appropriately.
Importance of Healthy Heart Valves
Healthy heart valves are vital for maintaining the overall function of the cardiovascular system. They ensure that oxygen-rich blood is delivered to the body’s organs and tissues while carbon dioxide and other waste products are efficiently removed. When heart valves are compromised, the heart has to work harder to pump blood, which can lead to heart failure, arrhythmias, and other serious conditions.
Heart valve disease can be congenital, meaning it is present at birth, or acquired due to factors such as infections, age-related changes, or other underlying health conditions. Early detection and appropriate treatment are crucial to managing heart valve disease effectively and improving the patient’s quality of life.
This introduction sets the stage for understanding the complexities of heart valve disease, highlighting why awareness and timely intervention are critical.
Types of Heart Valve Disease
Heart valve disease can affect any of the four heart valves: the aortic, mitral, tricuspid, and pulmonary valves. Each valve has a unique role in the heart’s function, and when one of these valves is compromised, it can lead to specific types of heart valve disease. Understanding the different types of valve disease helps in identifying the appropriate treatment options and managing the condition effectively.
Aortic Valve Disease
The aortic valve controls blood flow from the heart’s left ventricle into the aorta, the main artery that delivers oxygenated blood to the body. Aortic valve disease primarily manifests in two forms: aortic stenosis and aortic regurgitation.
- Aortic Stenosis: This condition occurs when the aortic valve narrows, limiting blood flow from the heart into the aorta. It is often caused by calcification, congenital valve defects, or rheumatic fever. Aortic stenosis can lead to symptoms such as chest pain, fainting, and shortness of breath.
- Aortic Regurgitation: In this condition, the aortic valve does not close properly, causing blood to flow backward into the left ventricle. This backflow forces the heart to work harder, which can eventually lead to heart failure. Common causes include valve degeneration, high blood pressure, and infections such as endocarditis.
Mitral Valve Disease
The mitral valve regulates blood flow between the left atrium and the left ventricle. It is one of the most commonly affected valves in heart valve disease.
- Mitral Stenosis: Mitral stenosis occurs when the mitral valve becomes narrowed, restricting blood flow from the left atrium to the left ventricle. This condition is often caused by rheumatic fever and can lead to symptoms like fatigue, irregular heartbeats, and difficulty breathing, especially during physical exertion.
- Mitral Regurgitation: This condition arises when the mitral valve does not close tightly, allowing blood to leak backward into the left atrium. Mitral regurgitation can result from mitral valve prolapse, damage from a heart attack, or other conditions that stretch or damage the valve tissues. Symptoms may include heart palpitations, swelling in the legs, and fluid buildup in the lungs.
Tricuspid Valve Disease
The tricuspid valve regulates blood flow between the right atrium and the right ventricle. Though less common, tricuspid valve disease can still significantly impact heart function.
- Tricuspid Stenosis: This rare condition involves narrowing of the tricuspid valve, often due to rheumatic fever or congenital defects. It restricts blood flow into the right ventricle, causing symptoms like abdominal swelling and liver enlargement.
- Tricuspid Regurgitation: Occurs when the tricuspid valve fails to close properly, allowing blood to flow back into the right atrium. Causes include heart failure, pulmonary hypertension, or damage from infections. Symptoms often include fatigue, swelling, and a pulsating neck vein.
Pulmonary Valve Disease
The pulmonary valve controls blood flow from the right ventricle to the pulmonary arteries, which carry blood to the lungs for oxygenation.
- Pulmonary Stenosis: A condition where the pulmonary valve is narrowed, often due to congenital heart defects. This restriction forces the heart to work harder to pump blood to the lungs, leading to symptoms like heart murmurs, chest pain, and cyanosis (bluish skin).
- Pulmonary Regurgitation: In this condition, the pulmonary valve does not close properly, causing blood to flow back into the right ventricle. It is commonly associated with conditions like pulmonary hypertension and can lead to right-sided heart failure if left untreated.
Understanding the specific type of valve disease is crucial for tailoring the right treatment approach, whether it be surgical, medical, or lifestyle interventions.
Causes of Heart Valve Disease
Heart valve disease can develop due to various factors, ranging from congenital defects present at birth to conditions acquired later in life. Understanding the causes of heart valve disease is essential for both prevention and treatment, as it allows for targeted interventions that can improve patient outcomes.
Congenital Heart Defects
Congenital heart defects are among the most common causes of heart valve disease. These defects are present at birth and occur when the heart valves do not form correctly during fetal development. Examples include bicuspid aortic valve, where the aortic valve has only two cusps instead of the usual three, making it more prone to stenosis or regurgitation. Other congenital defects can involve abnormal connections between the chambers of the heart, leading to increased stress on the valves and eventually causing them to malfunction.
Age-Related Changes
As individuals age, the heart valves can become thicker and stiffer, leading to a decline in their functionality. Calcification, a condition where calcium deposits build up on the valve leaflets, is particularly common in older adults. This buildup can cause the valves to stiffen and narrow, leading to conditions like aortic stenosis. Additionally, wear and tear over time can weaken the valve structures, making them less capable of closing properly, which can result in regurgitation.
Infections and Other Medical Conditions
Infections are a significant risk factor for heart valve disease. Rheumatic fever, which can develop after an untreated streptococcal throat infection, can cause inflammation and scarring of the heart valves, leading to conditions such as mitral stenosis. Although less common in developed countries due to widespread use of antibiotics, it remains a major cause of valve disease in parts of the world where healthcare access is limited.
Endocarditis, an infection of the inner lining of the heart chambers and valves, can also severely damage the heart valves. It typically occurs when bacteria or other pathogens enter the bloodstream and lodge on the heart valves, leading to infection and subsequent damage. This condition can affect any heart valve and often requires prompt medical treatment to prevent severe complications.
Other medical conditions, such as high blood pressure, heart failure, and connective tissue disorders like Marfan syndrome, can also contribute to the development of heart valve disease. High blood pressure, for instance, increases the workload on the heart, which can cause the valve leaflets to thicken and function improperly over time.
Radiation Therapy
Radiation therapy to the chest, used to treat cancers such as lymphoma or breast cancer, can sometimes damage the heart valves. This damage may not become apparent until many years after the treatment, as the radiation can cause fibrosis or thickening of the valve tissues, leading to stenosis or regurgitation.
Lifestyle Factors
Although not direct causes, certain lifestyle factors can increase the risk of developing heart valve disease. Smoking, poor diet, and lack of exercise contribute to conditions like hypertension and atherosclerosis, which in turn can stress the heart valves and impair their function. Additionally, obesity and diabetes are associated with an increased risk of heart valve disease due to their impact on overall cardiovascular health.
Genetic Predisposition
Some individuals may have a genetic predisposition to developing heart valve disease. Family history of heart valve problems can indicate a higher risk, particularly for conditions like bicuspid aortic valve or other congenital abnormalities. Genetic testing and regular monitoring may be recommended for those with a family history of heart valve disease to ensure early detection and intervention.
Understanding these causes allows healthcare providers to better assess risk factors and implement strategies to prevent or mitigate the progression of heart valve disease, improving patient outcomes through timely and appropriate care.
Symptoms of Heart Valve Disease
The symptoms of heart valve disease can vary widely depending on the specific valve affected, the severity of the disease, and the individual’s overall health. Some people may experience significant symptoms early on, while others may not notice any signs until the disease has progressed. Recognizing these symptoms is crucial for early diagnosis and treatment, which can prevent further complications and improve the quality of life.
Common Symptoms
Heart valve disease often manifests through a range of symptoms, many of which are related to the heart’s diminished ability to pump blood efficiently. Common symptoms include:
- Shortness of Breath: One of the most prevalent symptoms, shortness of breath can occur during physical activity or even at rest. This happens because the heart struggles to maintain adequate blood flow, leading to congestion in the lungs.
- Fatigue and Weakness: As the heart’s efficiency declines, less oxygen-rich blood reaches the muscles and tissues, resulting in persistent tiredness and a lack of energy. This can significantly impact daily activities and overall quality of life.
- Chest Pain or Discomfort: Particularly common in aortic valve disease, chest pain or tightness often occurs during physical exertion when the heart needs to work harder. This pain, known as angina, results from reduced blood flow to the heart muscle itself.
- Heart Palpitations: Patients may experience palpitations, or the sensation that the heart is racing, fluttering, or beating irregularly. This is often due to the heart’s efforts to compensate for faulty valves, leading to arrhythmias.
- Swelling (Edema): Fluid retention is another common symptom, particularly in the legs, ankles, feet, or abdomen. This occurs because poor blood flow causes fluid to leak from the blood vessels into surrounding tissues.
- Dizziness or Fainting: A reduction in blood flow due to valve disease can cause dizziness, lightheadedness, or even fainting spells, especially when standing up quickly or engaging in physical activity. This is more frequently seen in conditions like aortic stenosis.
How Symptoms Vary by Valve Type
The specific symptoms of heart valve disease can vary depending on which valve is affected:
- Aortic Valve Disease: Common symptoms include chest pain, shortness of breath, and fainting, particularly during exertion. Aortic stenosis often leads to noticeable symptoms as the condition progresses due to the valve’s critical role in pumping blood to the entire body.
- Mitral Valve Disease: Mitral valve regurgitation and stenosis can cause shortness of breath, fatigue, and heart palpitations. In severe cases, fluid buildup in the lungs (pulmonary edema) can occur, leading to coughing and difficulty breathing, especially when lying down.
- Tricuspid Valve Disease: Symptoms often include swelling in the legs, abdomen, and neck veins, due to the valve’s impact on blood flow returning from the body to the heart. This can lead to a feeling of fullness or bloating in the abdomen.
- Pulmonary Valve Disease: This condition may cause shortness of breath, fatigue, and a bluish tint to the skin (cyanosis) due to insufficient blood flow to the lungs for oxygenation. Pulmonary valve issues are less common but can still significantly impact heart function.
Silent Progression and Sudden Onset
It’s important to note that heart valve disease can progress silently, with minimal or no symptoms for a long time. This is particularly true in cases of mild regurgitation or stenosis, where the heart compensates for the reduced efficiency of the valves. However, as the disease progresses, symptoms can suddenly become severe.
In some cases, the onset of symptoms can be rapid and severe, requiring immediate medical attention. This is particularly true for acute conditions like sudden valve rupture due to infection or other causes. Patients experiencing sudden severe symptoms such as intense chest pain, extreme shortness of breath, or fainting should seek emergency care.
Early recognition of these symptoms and regular check-ups are essential, especially for individuals with known risk factors or a history of heart valve problems. Early intervention can significantly improve the prognosis and help manage the disease effectively.
Diagnosis of Heart Valve Disease
Diagnosing heart valve disease accurately is crucial for determining the appropriate treatment strategy. Early and precise diagnosis can help prevent the progression of the disease and reduce the risk of complications such as heart failure or arrhythmias. The diagnosis process typically involves a combination of a physical examination, patient history, and various diagnostic tests.
Physical Examination
The initial step in diagnosing heart valve disease often involves a thorough physical examination conducted by a healthcare provider. During this exam, the doctor listens to the patient’s heart using a stethoscope. One of the key indicators of valve disease is the presence of a heart murmur, which is an abnormal sound caused by turbulent blood flow through a faulty valve. While not all murmurs indicate valve disease, they often prompt further investigation.
In addition to listening for murmurs, the doctor may check for signs of fluid retention, such as swelling in the legs or abdomen, which could indicate that the heart is not pumping blood efficiently. The presence of irregular heartbeats or other abnormal heart sounds may also suggest issues with the heart valves.
Diagnostic Tests
To confirm the presence and extent of heart valve disease, doctors use a variety of diagnostic tests. These tests provide detailed information about the structure and function of the heart valves, helping to identify which valve is affected and the severity of the disease.
- EchocardiogramThe echocardiogram is one of the most common and informative tests used in diagnosing heart valve disease. It uses ultrasound waves to create detailed images of the heart’s structure and function. There are different types of echocardiograms:
- Transthoracic Echocardiogram (TTE): This non-invasive test involves placing a transducer on the chest to send and receive sound waves, producing images of the heart. It helps assess the size and shape of the heart, valve motion, and blood flow through the heart.
- Transesophageal Echocardiogram (TEE): In this procedure, a small transducer is passed down the esophagus, which lies close to the heart. This provides clearer images of the heart valves, particularly useful when TTE results are inconclusive or when more detailed imaging is needed.
- Electrocardiogram (ECG or EKG)An electrocardiogram measures the electrical activity of the heart and helps identify irregular heart rhythms (arrhythmias) that may be associated with valve disease. While an ECG does not directly visualize the heart valves, it provides valuable information about the heart’s overall function.
- Chest X-rayA chest X-ray can provide visual clues about the size and shape of the heart and detect any changes that might indicate heart valve disease, such as an enlarged heart or fluid buildup in the lungs. It also helps rule out other conditions that could be causing symptoms.
- Cardiac MRIMagnetic Resonance Imaging (MRI) of the heart offers detailed images of the heart’s structure and function. It is particularly useful for assessing the severity of valve disease and the impact on heart chambers. MRI can provide more precise measurements of blood flow and heart valve movement compared to other imaging methods.
- CT ScanA cardiac CT scan uses X-rays to create detailed cross-sectional images of the heart. It is often used to evaluate the aortic valve and aorta, especially in preparation for certain procedures like transcatheter aortic valve replacement (TAVR). CT scans are valuable for visualizing calcium deposits on valves, which can affect their function.
- Cardiac CatheterizationCardiac catheterization is an invasive procedure that provides detailed information about the heart’s blood flow and pressure. During this procedure, a thin tube (catheter) is inserted into a blood vessel and guided to the heart. Contrast dye is injected, allowing X-ray images of the heart and blood vessels. This test is particularly useful for evaluating the severity of valve disease and determining whether surgical intervention is needed.
- Stress TestsStress tests assess how the heart performs under physical stress, usually through exercise or medication that stimulates the heart. These tests help evaluate the impact of valve disease on the heart’s function during increased activity and can identify symptoms that are not present at rest.
Interpreting the Results
Once all necessary tests are completed, the healthcare provider will review the results to determine the type and severity of heart valve disease. This information is critical for developing an effective treatment plan, which may include medications, lifestyle changes, or surgical interventions.
Early and accurate diagnosis of heart valve disease allows for timely treatment and better management of the condition, potentially improving outcomes and quality of life for patients.
Treatment Options for Heart Valve Disease
Treatment for heart valve disease depends on the specific valve affected, the severity of the disease, and the overall health of the patient. The primary goals of treatment are to improve symptoms, prevent complications, and enhance the quality of life. Treatment options range from lifestyle modifications and medications to surgical and non-surgical interventions.
Medication Management
Medications are often the first line of treatment for managing the symptoms of heart valve disease. While medications cannot cure valve disease, they can help manage symptoms and prevent complications. Common medications include:
- Diuretics: Also known as water pills, diuretics help reduce fluid buildup in the body, alleviating symptoms such as swelling in the legs and lungs. This can be particularly helpful for patients with valve diseases that lead to heart failure or fluid retention.
- Beta-blockers: These medications help reduce the heart rate and blood pressure, easing the heart’s workload. Beta-blockers are commonly used in patients with aortic or mitral valve disease to manage symptoms like chest pain and palpitations.
- ACE Inhibitors and ARBs: Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) help relax blood vessels and lower blood pressure, making it easier for the heart to pump blood. These drugs are often prescribed for patients with regurgitation, where the heart needs to work harder to pump blood efficiently.
- Anticoagulants: Blood thinners, such as warfarin or newer anticoagulants, are used to prevent blood clots in patients with certain types of valve disease, particularly those with atrial fibrillation or artificial valve replacements. Anticoagulants help reduce the risk of stroke or other clot-related complications.
Surgical Interventions
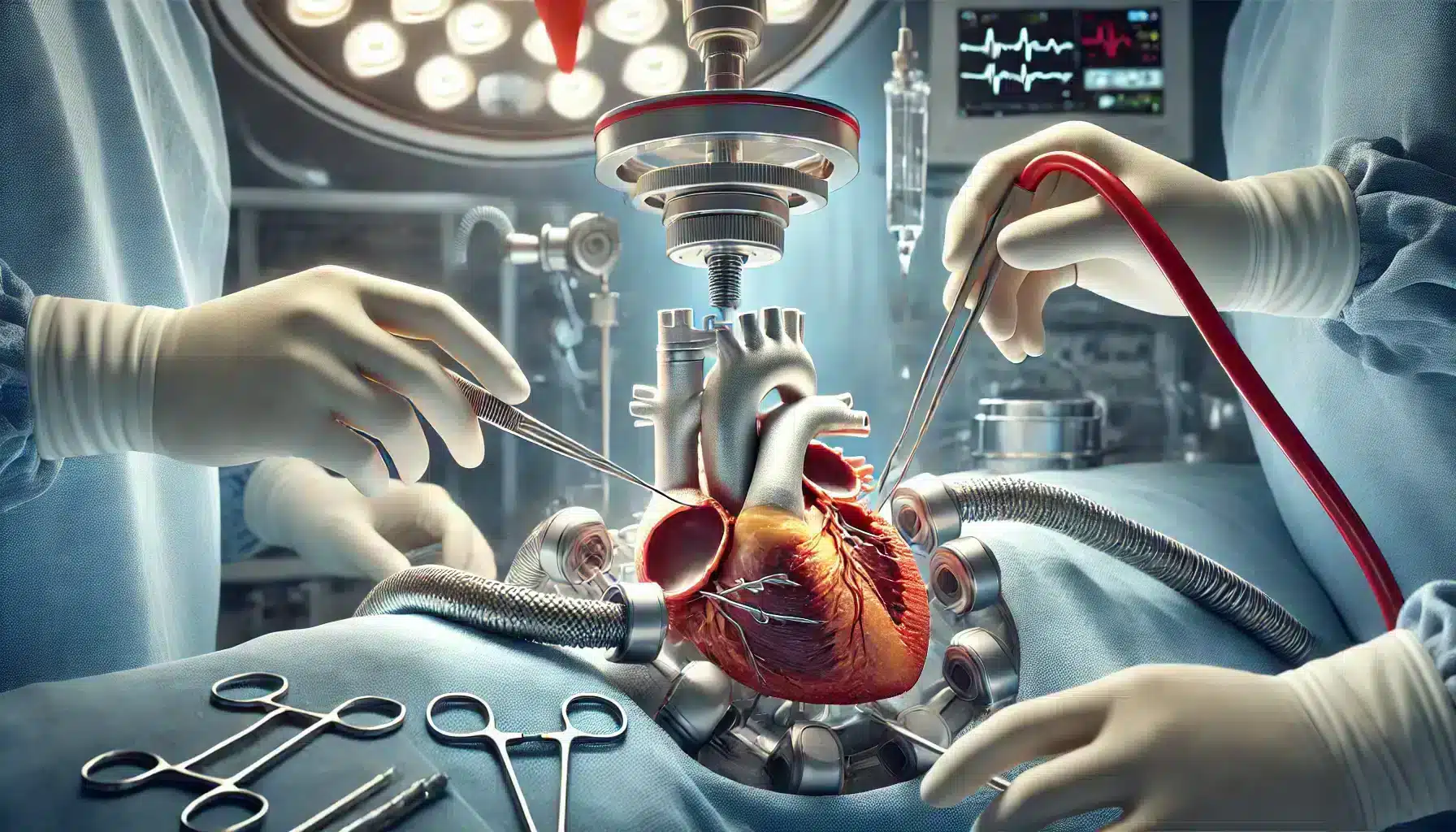
When heart valve disease progresses to a severe stage, surgical intervention may be necessary to repair or replace the affected valve. Surgical options are determined based on the specific condition, patient’s age, overall health, and other individual factors.
- Valve Repair: Valve repair involves procedures that restore the valve’s normal function without replacing it. Repair techniques include reshaping the valve leaflets, removing excess tissue, or tightening the ring around the valve (annuloplasty). Valve repair is often preferred over replacement when feasible, as it preserves the patient’s natural valve and typically results in better long-term outcomes.
- Valve Replacement: When valve repair is not possible or effective, valve replacement surgery may be recommended. There are two main types of replacement valves:
- Mechanical Valves: Made of durable materials such as metal or ceramic, mechanical valves can last a lifetime. However, patients with mechanical valves need to take lifelong anticoagulant medications to prevent blood clots.
- Biological Valves: These valves are made from animal tissues (bovine or porcine) or human donor valves. Biological valves do not require lifelong anticoagulation, but they tend to wear out over time and may need to be replaced after 10-20 years.
- Open-Heart Surgery: Traditional valve repair or replacement surgery is typically performed through open-heart surgery, where the chest is opened, and the heart is temporarily stopped. While this is an invasive procedure, it is highly effective in treating severe valve disease.
Non-Surgical Procedures
Advancements in medical technology have led to the development of less invasive procedures for treating heart valve disease, offering alternatives to traditional open-heart surgery.
- Balloon Valvuloplasty: This procedure is used primarily to treat stenosis, particularly in the aortic, mitral, or pulmonary valves. A catheter with a balloon at its tip is inserted through a blood vessel and guided to the narrowed valve. The balloon is then inflated to widen the valve opening, improving blood flow. While effective, the results of balloon valvuloplasty may not be permanent, and the procedure may need to be repeated.
- Transcatheter Aortic Valve Replacement (TAVR): TAVR is a minimally invasive procedure used to replace the aortic valve without open-heart surgery. A new valve is inserted via a catheter through a small incision, usually in the groin, and guided to the heart. TAVR is especially beneficial for patients who are at high risk for traditional surgery due to age or other health conditions.
- MitraClip: For patients with mitral regurgitation who are not candidates for surgery, a MitraClip procedure can be performed. A small clip is attached to the mitral valve via a catheter, allowing the valve to close more completely and reduce regurgitation.
Lifestyle Modifications
In addition to medical and surgical treatments, lifestyle changes play a crucial role in managing heart valve disease. These modifications can help reduce symptoms and improve overall heart health:
- Diet and Exercise: Maintaining a heart-healthy diet low in salt, saturated fats, and cholesterol can help manage blood pressure and reduce the strain on the heart. Regular physical activity, as recommended by a healthcare provider, can improve cardiovascular fitness and overall well-being.
- Smoking Cessation: Smoking is a major risk factor for cardiovascular disease, including heart valve disease. Quitting smoking can significantly improve heart health and reduce the risk of complications.
- Weight Management: Maintaining a healthy weight can reduce the burden on the heart and help manage symptoms like shortness of breath and fatigue.
Ongoing Monitoring and Care
Patients with heart valve disease require regular follow-up appointments with their healthcare provider to monitor the condition of their valves and overall heart function. This includes routine echocardiograms, physical exams, and possibly other tests to assess the progression of the disease. Early detection of changes in valve function can allow for timely adjustments to the treatment plan, potentially preventing the need for more invasive interventions.
Living with Heart Valve Disease
Living with heart valve disease requires ongoing management and lifestyle adjustments to maintain heart health and quality of life. While treatment options such as medications, surgeries, and minimally invasive procedures can significantly improve symptoms and prognosis, the day-to-day management of the condition plays a crucial role in long-term outcomes. This section covers key strategies for living well with heart valve disease, including lifestyle modifications, regular monitoring, and mental health considerations.
Lifestyle Modifications
Adopting heart-healthy lifestyle habits is essential for managing heart valve disease and reducing the risk of complications. These modifications can help alleviate symptoms, slow disease progression, and improve overall well-being.
- Healthy Diet: A heart-healthy diet is low in saturated fats, trans fats, cholesterol, and sodium. Emphasizing fruits, vegetables, whole grains, lean proteins, and healthy fats can help manage blood pressure, cholesterol levels, and weight. Reducing sodium intake is particularly important for patients with heart valve disease, as it helps prevent fluid retention and reduces the strain on the heart.
- Regular Physical Activity: Staying active is beneficial for heart health, but it’s important to tailor physical activity to individual capabilities and the severity of the valve disease. Low to moderate-intensity exercises, such as walking, swimming, or cycling, are generally recommended. However, patients should consult their healthcare provider before starting any new exercise regimen to ensure it is safe and appropriate.
- Smoking Cessation: Smoking is a significant risk factor for cardiovascular disease, and quitting smoking is one of the most effective ways to improve heart health. Smoking cessation can help reduce the progression of valve disease and lower the risk of other heart-related complications.
- Weight Management: Maintaining a healthy weight can reduce the workload on the heart and help manage symptoms like shortness of breath and fatigue. Weight loss, when needed, should be approached gradually and with the guidance of a healthcare provider or dietitian to ensure it is done safely and sustainably.
- Alcohol Moderation: Excessive alcohol consumption can worsen heart valve disease symptoms and lead to other cardiovascular issues. Patients are advised to limit alcohol intake or avoid it altogether, especially if they are taking medications that interact negatively with alcohol.
Ongoing Monitoring and Follow-Up Care
Regular monitoring and follow-up care are critical for managing heart valve disease effectively. Patients should adhere to their scheduled appointments with their cardiologist or primary care provider to monitor the condition of their heart valves and overall heart function.
- Routine Tests: Regular echocardiograms are often recommended to assess the function of the heart valves and detect any changes in valve structure or performance. Additional tests such as stress tests, EKGs, or cardiac MRIs may be ordered based on the patient’s specific condition and symptoms.
- Medication Adherence: It is essential for patients to take prescribed medications exactly as directed to manage symptoms and prevent complications. This includes medications for blood pressure control, anticoagulants to prevent blood clots, or any other medications prescribed as part of the treatment plan.
- Symptom Awareness: Patients should be vigilant about monitoring their symptoms and report any changes to their healthcare provider promptly. Worsening symptoms such as increased shortness of breath, chest pain, or swelling could indicate a change in the severity of the valve disease and may require adjustments to the treatment plan.
Mental and Emotional Health
Living with a chronic condition like heart valve disease can be challenging, and it’s important to address mental and emotional health as part of overall care. Patients may experience anxiety, depression, or stress related to their diagnosis, treatment, or the impact of the disease on their daily lives.
- Support Systems: Building a strong support network can provide emotional comfort and practical assistance. This can include family, friends, support groups, or counseling services. Connecting with others who have similar experiences can help patients feel understood and less isolated.
- Stress Management: Stress can negatively impact heart health, so finding effective ways to manage stress is important. Techniques such as deep breathing exercises, meditation, yoga, or engaging in hobbies can help reduce stress levels and improve overall well-being.
- Education and Empowerment: Being well-informed about heart valve disease empowers patients to make proactive decisions about their health. Understanding their condition, treatment options, and the importance of lifestyle changes can help patients take control of their health and feel more confident in managing their disease.
Preventing Complications
Proactive management of heart valve disease also involves steps to prevent complications, such as heart failure, stroke, or infective endocarditis. Patients should follow their healthcare provider’s advice on preventive measures, which may include:
- Endocarditis Prevention: Patients with certain types of valve disease or those who have had valve replacement surgery may be at higher risk for infective endocarditis, an infection of the heart valves. Preventive measures include maintaining good oral hygiene, avoiding body piercings or tattoos, and taking antibiotics before certain medical or dental procedures as recommended by their healthcare provider.
- Risk Factor Management: Controlling other cardiovascular risk factors, such as high blood pressure, high cholesterol, and diabetes, is essential for reducing the overall strain on the heart and preventing further complications. Regular check-ups and appropriate medication adjustments are critical for managing these conditions effectively.
Living with heart valve disease requires a comprehensive approach that includes medical management, lifestyle changes, regular monitoring, and attention to mental and emotional well-being. With proper care and proactive management, many patients can lead full and active lives despite their diagnosis.
Prevention and Risk Management
While some forms of heart valve disease, such as congenital defects, cannot be prevented, there are several strategies that can help reduce the risk of developing acquired heart valve disease or slow its progression. Prevention and risk management focus on maintaining overall heart health, managing risk factors, and adopting healthy lifestyle habits.
Preventive Measures
1. Manage Blood Pressure and Cholesterol Levels
High blood pressure and high cholesterol are significant risk factors for heart valve disease, as they can lead to calcification and damage to the valves over time. Managing these conditions through lifestyle changes and, if necessary, medications can significantly reduce the risk of developing valve disease.
- Blood Pressure Control: Regular monitoring and maintaining a healthy blood pressure level (typically below 120/80 mmHg) can help reduce strain on the heart and prevent damage to the valves. Patients should follow a low-sodium diet, exercise regularly, and take antihypertensive medications as prescribed.
- Cholesterol Management: High levels of LDL (bad) cholesterol can contribute to the buildup of plaque and calcification on heart valves. A heart-healthy diet, rich in fiber and low in saturated fats, along with cholesterol-lowering medications if needed, can help keep cholesterol levels in check.
2. Prevent and Manage Infections
Infections such as rheumatic fever and infective endocarditis can cause significant damage to heart valves. Preventing these infections through proper medical care and preventive measures is critical.
- Rheumatic Fever Prevention: Prompt treatment of strep throat with antibiotics can prevent rheumatic fever, which can lead to valve damage, particularly the mitral valve. Ensuring complete treatment of streptococcal infections is crucial, especially in children and adolescents.
- Infective Endocarditis Prevention: Patients at high risk for endocarditis, such as those with existing valve disease or prosthetic valves, should take antibiotics before certain dental and medical procedures to prevent bacteria from entering the bloodstream. Maintaining good oral hygiene and avoiding high-risk activities, like getting tattoos or piercings, can also reduce the risk.
3. Maintain a Healthy Lifestyle
Adopting a heart-healthy lifestyle is one of the most effective ways to prevent heart valve disease and manage risk factors. Key components include:
- Balanced Diet: Eating a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats helps support heart health and manage weight, blood pressure, and cholesterol levels.
- Regular Physical Activity: Engaging in regular exercise, such as brisk walking, swimming, or cycling, helps maintain cardiovascular fitness and reduce the risk of heart disease. Patients should aim for at least 150 minutes of moderate exercise per week, but should consult with their healthcare provider to tailor exercise recommendations to their specific condition.
- Avoid Smoking and Limit Alcohol: Smoking damages blood vessels and the heart, increasing the risk of heart valve disease and other cardiovascular conditions. Quitting smoking is one of the most effective preventive measures. Limiting alcohol intake also helps maintain heart health and prevent complications.
4. Monitor and Manage Other Health Conditions
Managing other health conditions that can contribute to heart valve disease is essential for risk reduction. This includes controlling diabetes, obesity, and other cardiovascular conditions that can exacerbate valve problems.
- Diabetes Management: Keeping blood sugar levels under control through diet, exercise, and medications as prescribed can help prevent complications that might contribute to heart valve disease.
- Obesity Management: Maintaining a healthy weight reduces the strain on the heart and lowers the risk of developing cardiovascular problems. Weight loss strategies should focus on sustainable, healthy changes rather than quick fixes.
Risk Factor Management
1. Genetic Risk Factors
While some individuals have a genetic predisposition to heart valve disease, particularly congenital forms like bicuspid aortic valve, knowing family history can help guide preventive care. For those with a family history of valve disease, regular monitoring and early intervention are key to managing risks effectively.
2. Age-Related Risks
Aging is a significant risk factor for heart valve disease, as valves can thicken, calcify, and lose flexibility over time. Although aging cannot be prevented, maintaining overall heart health through a balanced diet, regular exercise, and regular medical check-ups can help mitigate age-related risks.
3. Monitoring and Regular Check-ups
Regular medical check-ups, including heart evaluations and imaging tests such as echocardiograms, are important for early detection of changes in valve function. Early diagnosis and timely treatment can prevent the progression of valve disease and reduce the likelihood of severe complications.
4. Educating and Empowering Patients
Education plays a crucial role in prevention and risk management. Patients who are well-informed about heart valve disease and its risk factors are more likely to take proactive steps to maintain their heart health. Healthcare providers should emphasize the importance of lifestyle modifications, adherence to prescribed treatments, and regular monitoring to empower patients in managing their condition.
Prevention and risk management strategies are essential for reducing the burden of heart valve disease and improving patient outcomes. By focusing on heart-healthy habits, managing risk factors, and staying vigilant with regular monitoring, individuals can significantly lower their risk of developing or worsening heart valve disease.
Future of Heart Valve Disease Treatment
The treatment of heart valve disease has evolved significantly over the years, with advancements in medical technology and surgical techniques providing better outcomes and less invasive options for patients. The future of heart valve disease treatment looks promising, with ongoing research and innovations poised to further enhance the management and care of this condition. This section explores some of the latest advancements and emerging trends that are shaping the future of heart valve disease treatment.
Advances in Treatment Technologies
1. Minimally Invasive Procedures
Minimally invasive procedures have revolutionized the treatment of heart valve disease, offering alternatives to traditional open-heart surgery with reduced recovery times and lower risk of complications. The development of transcatheter techniques has been particularly impactful, making valve replacement and repair accessible to a broader range of patients, including those who are considered high-risk for surgery.
- Transcatheter Aortic Valve Replacement (TAVR): TAVR has become a standard treatment for patients with aortic stenosis, especially those who are not candidates for conventional surgery. The procedure involves delivering a new valve via a catheter, usually through the femoral artery, and positioning it within the diseased aortic valve. As TAVR technology continues to advance, it is being considered for use in younger and lower-risk patients, expanding its applicability.
- Transcatheter Mitral Valve Repair and Replacement: Similar to TAVR, transcatheter techniques for the mitral valve, such as MitraClip for mitral regurgitation, are gaining traction. Research and development efforts are focused on creating new devices and refining existing ones to improve outcomes for patients with mitral valve disease.
- Percutaneous Pulmonary Valve Replacement: For patients with pulmonary valve disease, percutaneous approaches allow for valve replacement without open-heart surgery. These procedures are particularly beneficial for patients with congenital heart defects who require multiple interventions over their lifetime.
2. Bioprosthetic Valve Durability Improvements
Bioprosthetic valves, made from animal tissue, are widely used due to their lower risk of blood clot formation compared to mechanical valves. However, their durability has been a concern, as they typically last 10-20 years before needing replacement. Research is underway to improve the longevity of bioprosthetic valves, with advancements in tissue engineering and valve preservation techniques showing promise in extending their lifespan.
3. Personalized and Precision Medicine
The future of heart valve disease treatment is likely to include more personalized approaches, where treatment plans are tailored to the individual characteristics of each patient. This could involve genetic testing to identify patients at risk for certain types of valve disease or to guide the selection of the most appropriate treatment. Advances in imaging technology also allow for more precise assessment of valve anatomy and function, enabling highly individualized treatment strategies.
4. Valve-in-Valve Procedures
Valve-in-valve procedures involve placing a new valve inside a previously implanted prosthetic valve that has failed. This approach provides a less invasive option for patients who have already undergone valve replacement and need a second intervention. Valve-in-valve procedures are increasingly used in cases where traditional reoperation would be high-risk, offering a safer and effective alternative.
Ongoing Research and Clinical Trials
1. Development of Next-Generation Valves
Research continues into the development of next-generation heart valves that combine the best features of mechanical and bioprosthetic valves. These valves aim to provide long-term durability without the need for lifelong anticoagulation therapy, addressing a major limitation of current valve options. Innovative materials, such as polymers and hybrid designs, are being explored to achieve this goal.
2. Stem Cell and Regenerative Therapies
Regenerative medicine holds the potential to transform heart valve disease treatment by enabling the repair or replacement of damaged heart tissue using the body’s own cells. Stem cell therapies are being investigated for their ability to regenerate heart valve tissues, potentially offering a solution that goes beyond conventional repair or replacement. While still in the experimental stages, these therapies represent a promising frontier in heart valve disease treatment.
3. Anticoagulation Alternatives
For patients with mechanical valves, the need for lifelong anticoagulation therapy poses a significant challenge due to the risk of bleeding complications. Research is focused on developing alternative anticoagulation strategies, including novel oral anticoagulants that are safer and more convenient than traditional medications like warfarin. Additionally, advances in valve design may reduce the need for anticoagulation altogether.
4. Remote Monitoring and Digital Health Tools
The integration of digital health tools, such as wearable devices and remote monitoring systems, is expected to play an increasingly important role in the management of heart valve disease. These technologies allow for continuous monitoring of heart function and symptoms, enabling early detection of changes that may require intervention. Remote monitoring also facilitates better communication between patients and healthcare providers, supporting more proactive and personalized care.
5. Artificial Intelligence and Machine Learning
Artificial intelligence (AI) and machine learning are being leveraged to improve the diagnosis and treatment of heart valve disease. AI algorithms can analyze large volumes of imaging data to identify subtle changes in valve function that may be missed by the human eye. Machine learning models are also being developed to predict patient outcomes and guide treatment decisions, enhancing the precision and effectiveness of care.
The Future of Patient Care
As technology continues to advance, the future of heart valve disease treatment will likely be characterized by less invasive procedures, longer-lasting valves, and more personalized care strategies. These innovations have the potential to significantly improve patient outcomes, reduce recovery times, and expand treatment options for those previously considered inoperable. Ongoing research and clinical trials will be crucial in bringing these new therapies to the forefront of heart valve disease management, ensuring that patients receive the best possible care.
Conclusion
Heart valve disease is a complex condition that affects millions of people worldwide, presenting a variety of challenges in diagnosis, treatment, and long-term management. However, advancements in medical technology, surgical techniques, and personalized care have significantly improved the outlook for patients with heart valve disease. From minimally invasive procedures like TAVR and MitraClip to cutting-edge research in regenerative medicine and artificial intelligence, the future of heart valve disease treatment is brighter than ever.
Early detection and proactive management are key to improving outcomes for patients with heart valve disease. Regular check-ups, a heart-healthy lifestyle, and adherence to prescribed treatments can help manage symptoms, slow disease progression, and prevent complications. For those who require surgical intervention, the availability of less invasive options offers a path to recovery with fewer risks and faster healing times.
As we look to the future, ongoing research and innovation promise to further refine the ways we diagnose, treat, and manage heart valve disease. The development of next-generation valves, personalized treatment strategies, and advanced monitoring tools will continue to enhance patient care, making it possible for more individuals to lead full and active lives despite their diagnosis.
Patients are encouraged to stay informed about their condition, work closely with their healthcare providers, and take an active role in managing their heart health. With the right combination of medical care, lifestyle adjustments, and support, living well with heart valve disease is not only possible but achievable.
In summary, heart valve disease, while serious, is a condition that can be effectively managed with current and emerging treatment options. By embracing the latest advancements and maintaining a proactive approach to heart health, patients can look forward to better outcomes and an improved quality of life.