Understanding Sleep Apnea: An Overview
How Sleep Apnea Affects Heart Failure? Sleep apnea is a common sleep disorder characterized by repeated interruptions in breathing during sleep. These interruptions, known as apneas, can occur multiple times throughout the night, leading to poor sleep quality and various health complications. There are two primary types of sleep apnea: obstructive sleep apnea (OSA) and central sleep apnea (CSA). OSA is the most prevalent form and occurs when the throat muscles intermittently relax and block the airway during sleep. In contrast, CSA is related to the brain’s inability to send proper signals to the muscles that control breathing.
Individuals with sleep apnea often experience symptoms such as loud snoring, gasping for air during sleep, excessive daytime sleepiness, and morning headaches. The condition is more common in individuals who are overweight, older, or have a family history of sleep apnea.
Types of Sleep Apnea
- Obstructive Sleep Apnea (OSA): Caused by the relaxation of throat muscles, leading to blocked airways.
- Central Sleep Apnea (CSA): Occurs when the brain fails to send proper signals to the muscles that control breathing.
- Complex Sleep Apnea Syndrome: A combination of both OSA and CSA, also known as treatment-emergent central sleep apnea.
What is Heart Failure?
Heart failure is a chronic condition in which the heart is unable to pump sufficient blood to meet the body’s needs for blood and oxygen. It is often a result of other cardiovascular conditions such as coronary artery disease, high blood pressure, or diabetes. When the heart’s pumping action is weakened, blood flow slows down, and the heart becomes congested, causing fluid buildup in the lungs and other parts of the body.
There are several types of heart failure, categorized based on which side of the heart is affected or the condition’s progression. Left-sided heart failure is the most common and can lead to fluid accumulation in the lungs, causing shortness of breath. Right-sided heart failure, on the other hand, usually results in swelling in the legs and abdomen due to fluid retention.
Types of Heart Failure
- Left-Sided Heart Failure: This occurs when the left ventricle doesn’t pump efficiently, leading to fluid buildup in the lungs (pulmonary edema).
- Right-Sided Heart Failure: This type is characterized by the right side of the heart failing, causing fluid retention in the legs, feet, and abdomen.
- Congestive Heart Failure: A term often used to describe all types of heart failure, indicating fluid accumulation and congestion in the body’s tissues.

The Connection Between Sleep Apnea and Heart Failure
The relationship between sleep apnea and heart failure is complex and bidirectional. Sleep apnea can exacerbate heart failure, and conversely, heart failure can worsen sleep apnea symptoms. This connection primarily arises because sleep apnea increases the workload on the heart by causing intermittent drops in blood oxygen levels (hypoxia), frequent awakenings, and stress on the cardiovascular system.
During episodes of sleep apnea, the body reacts to the lack of oxygen by increasing heart rate and blood pressure. This places significant strain on the heart, especially in individuals already dealing with compromised heart function. Over time, the repetitive stress from untreated sleep apnea can lead to structural changes in the heart, worsening heart failure.
Mechanisms Linking Sleep Apnea and Heart Failure
- Intermittent Hypoxia: Repeated drops in blood oxygen levels during sleep can cause oxidative stress and inflammation, contributing to the progression of heart failure.
- Increased Sympathetic Activity: The body’s stress response is heightened during apneas, leading to increased heart rate and blood pressure, which can damage the heart over time.
- Negative Thoracic Pressure: Obstructive apneas cause negative pressure in the chest, increasing the workload on the heart and promoting fluid retention.

How Sleep Apnea Worsens Heart Failure
Sleep apnea contributes to the progression of heart failure through various physiological mechanisms. One of the primary ways it worsens heart failure is by disrupting normal sleep patterns, which are crucial for cardiovascular health. The repeated awakenings and poor sleep quality caused by apneas lead to increased sympathetic nervous system activity and elevated blood pressure, placing additional strain on the heart.
Furthermore, sleep apnea can lead to fluid shifts during sleep. When a person with sleep apnea lies down, fluid that accumulates in the legs during the day can move into the chest and neck, worsening airway obstruction and increasing the heart’s workload. This can exacerbate symptoms such as shortness of breath and fatigue, common in heart failure patients.
Impact on Blood Pressure and Heart Rhythm
- Hypertension: Sleep apnea frequently causes high blood pressure, which is a major risk factor for heart failure. The intermittent hypoxia and frequent arousals stimulate a persistent increase in blood pressure.
- Atrial Fibrillation: The stress and strain on the heart due to sleep apnea can lead to arrhythmias, particularly atrial fibrillation, which complicates heart failure management.
- Ventricular Dysfunction: Repeated apneas and hypoxia can lead to worsening of the heart’s pumping ability, exacerbating ventricular dysfunction in heart failure patients.
Symptoms of Sleep Apnea in Heart Failure Patients
Sleep apnea symptoms in heart failure patients can often be subtle and easily overlooked, yet they significantly impact the overall health and quality of life. Common symptoms include excessive daytime sleepiness, loud snoring, and abrupt awakenings accompanied by choking or gasping. These symptoms occur due to the repeated interruptions in breathing that disturb the sleep cycle and reduce oxygen levels in the blood.
For heart failure patients, additional symptoms may include worsening of heart failure symptoms such as increased shortness of breath, fatigue, and difficulty exercising. This is because the cardiovascular system is under continuous strain from the disrupted sleep patterns and oxygen deprivation caused by sleep apnea.
Common Signs to Watch For
- Loud Snoring: Persistent and loud snoring is a hallmark of obstructive sleep apnea and can be an early warning sign in heart failure patients.
- Daytime Fatigue: Due to fragmented sleep, patients often experience extreme tiredness during the day, which can exacerbate heart failure symptoms.
- Nighttime Awakenings: Frequent waking during the night with a feeling of breathlessness or choking is common in those with sleep apnea and heart failure.
Diagnosis and Screening for Sleep Apnea in Heart Failure Patients

Accurate diagnosis of sleep apnea in heart failure patients is critical for effective management and treatment of both conditions. Screening for sleep apnea typically involves a thorough evaluation of symptoms, a physical examination, and specialized sleep studies such as polysomnography. This comprehensive sleep test monitors various physiological parameters during sleep, including breathing patterns, heart rate, and blood oxygen levels, to identify sleep apnea.
For heart failure patients, home sleep apnea testing may also be considered, offering a more convenient and accessible option for diagnosis. It’s essential for healthcare providers to be vigilant in screening for sleep apnea in heart failure patients, as early detection can lead to better management and improved outcomes.
Screening Tools and Methods
- Polysomnography: A comprehensive overnight sleep study that records brain waves, blood oxygen levels, heart rate, and breathing to diagnose sleep apnea.
- Home Sleep Apnea Testing: A simplified test that can be done at home to monitor breathing and oxygen levels, making it more accessible for patients with heart failure.
- Epworth Sleepiness Scale: A questionnaire used to measure daytime sleepiness, which can help identify patients at risk for sleep apnea.
Treatment Options for Sleep Apnea in Heart Failure Patients
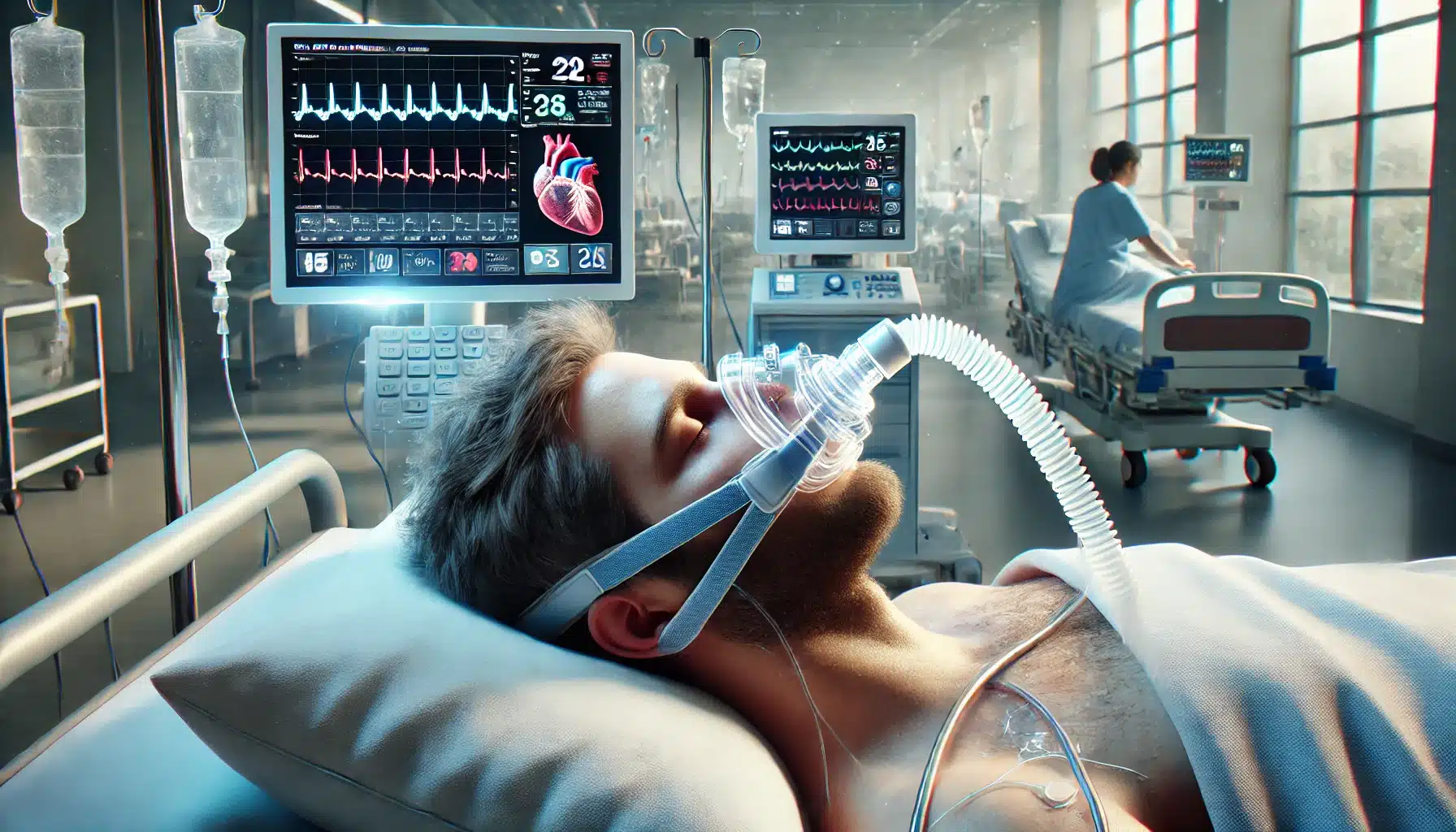
Treating sleep apnea in heart failure patients requires a multidisciplinary approach to address both conditions effectively. The primary goal of treatment is to improve breathing during sleep, enhance oxygenation, and reduce the strain on the heart. Common treatment options include Continuous Positive Airway Pressure (CPAP) therapy, lifestyle modifications, and in some cases, surgical interventions.
CPAP therapy is considered the gold standard for treating obstructive sleep apnea. It works by delivering a steady stream of air through a mask, keeping the airway open during sleep. This reduces apneas and improves sleep quality, which can have a significant positive impact on heart failure symptoms. In addition to CPAP, other treatments such as adaptive servo-ventilation and oxygen therapy may be used based on the patient’s specific needs.
Common Treatments and Therapies
- Continuous Positive Airway Pressure (CPAP): A device that uses mild air pressure to keep airways open, improving oxygen levels and reducing apneas during sleep.
- Bi-Level Positive Airway Pressure (BiPAP): Similar to CPAP but provides varying levels of air pressure for inhalation and exhalation, often used when CPAP is not tolerated.
- Adaptive Servo-Ventilation (ASV): A more advanced therapy that adjusts air pressure based on the patient’s breathing patterns, used particularly for central sleep apnea.

The Importance of Lifestyle Changes
In addition to medical treatments, lifestyle changes play a crucial role in managing both sleep apnea and heart failure. These modifications can help alleviate symptoms, improve overall health, and reduce the progression of both conditions. Common lifestyle changes include weight management, regular physical activity, and dietary adjustments.
Maintaining a healthy weight is particularly important, as excess weight can contribute to airway obstruction and worsen sleep apnea symptoms. Exercise, even at moderate levels, can improve cardiovascular fitness and help control heart failure symptoms. A heart-healthy diet, rich in fruits, vegetables, whole grains, and lean proteins, can further support cardiovascular health and reduce the impact of sleep apnea.
Effective Lifestyle Changes
- Weight Loss: Losing excess weight can significantly reduce the severity of sleep apnea and improve heart function in heart failure patients.
- Exercise: Regular physical activity helps strengthen the heart and improve overall cardiovascular health, which can benefit those with both sleep apnea and heart failure.
- Avoiding Alcohol and Smoking: Both alcohol and smoking can exacerbate sleep apnea symptoms and worsen heart failure, making avoidance crucial for management.
Preventive Measures and Management Tips
Preventing the onset or worsening of sleep apnea and heart failure involves proactive management strategies and adherence to treatment plans. Patients should work closely with healthcare providers to monitor their conditions and make necessary adjustments to their treatment regimens. Regular follow-ups, adherence to prescribed therapies, and lifestyle modifications are key components of effective management.
Preventive measures also include managing risk factors such as high blood pressure, diabetes, and obesity. Keeping these underlying conditions under control can significantly reduce the risk of developing or worsening sleep apnea and heart failure. Additionally, establishing good sleep hygiene practices, such as maintaining a regular sleep schedule and creating a comfortable sleep environment, can further help manage symptoms.
Key Management Tips
- Regular Monitoring: Consistently track symptoms and follow up with healthcare providers to ensure optimal management of both conditions.
- Adherence to Therapy: Strictly follow prescribed treatments, including CPAP therapy and medications, to control sleep apnea and support heart health.
- Manage Comorbidities: Control other health issues like hypertension and diabetes to reduce the impact on sleep apnea and heart failure.
FAQs About Sleep Apnea and Heart Failure
What are the main symptoms of sleep apnea in heart failure patients?
Common symptoms include loud snoring, excessive daytime sleepiness, abrupt awakenings with choking or gasping, and a general feeling of fatigue. In heart failure patients, these symptoms can also include worsening shortness of breath and difficulty exercising.
Can treating sleep apnea improve heart failure outcomes?
Yes, treating sleep apnea can significantly improve heart failure outcomes. Effective treatments like CPAP therapy can reduce the strain on the heart, improve sleep quality, and lower blood pressure, all of which contribute to better heart failure management.
What lifestyle changes can help manage both sleep apnea and heart failure?
Lifestyle changes such as maintaining a healthy weight, engaging in regular physical activity, avoiding alcohol and smoking, and following a heart-healthy diet can help manage both conditions. These changes reduce the severity of sleep apnea and support overall heart health.
Is sleep apnea common in heart failure patients?
Yes, sleep apnea is quite common in heart failure patients. The prevalence of sleep apnea in this group is significantly higher compared to the general population, making it crucial for heart failure patients to be screened and treated for sleep apnea.
How does sleep apnea affect blood pressure in heart failure patients?
Sleep apnea can cause frequent spikes in blood pressure during the night due to repeated oxygen deprivation and awakenings. This persistent increase in blood pressure adds strain to the heart and can worsen heart failure symptoms over time.