Understanding Heart Failure
Heart failure is a chronic condition where the heart is unable to pump blood efficiently enough to meet the body’s needs. This can lead to fatigue, shortness of breath, and other serious complications. The condition can affect one or both sides of the heart, and while it often develops gradually, it can also occur suddenly due to a major cardiac event. Understanding the underlying mechanisms of heart failure is crucial in managing the disease and improving the quality of life for patients.
There are several stages of heart failure, ranging from mild to severe, and the severity of the condition determines the approach to treatment. Early detection and intervention are essential in preventing the disease from progressing. In addition to medical treatments, lifestyle modifications such as diet and exercise play a pivotal role in managing heart failure.
- Stage A: High risk for heart failure, but no symptoms or structural heart disease present.
- Stage B: Structural heart disease present, but no symptoms of heart failure.
- Stage C: Structural heart disease with prior or current symptoms of heart failure.
- Stage D: Advanced heart failure requiring specialized interventions.
Causes and Types of Heart Failure
Heart failure can be caused by a variety of underlying health conditions that weaken or damage the heart over time. The most common causes include coronary artery disease, high blood pressure, diabetes, and previous heart attacks. Lifestyle factors such as smoking, poor diet, and lack of physical activity can also contribute to the development of heart failure.
There are two main types of heart failure: systolic heart failure and diastolic heart failure. Systolic heart failure occurs when the heart muscle becomes too weak to effectively pump blood. Diastolic heart failure, on the other hand, happens when the heart muscle becomes too stiff, preventing it from filling properly with blood between heartbeats.
- Systolic Heart Failure: This type of heart failure is characterized by the heart’s inability to contract forcefully enough to pump blood out of the heart chambers. It often leads to a reduced ejection fraction, meaning less blood is pumped out with each heartbeat.
- Diastolic Heart Failure: In this form, the heart’s ability to relax and fill with blood is impaired. Despite a normal ejection fraction, the heart is unable to accommodate the necessary amount of blood to meet the body’s demands.
Other classifications include left-sided heart failure, where the left ventricle fails, and right-sided heart failure, where the right ventricle struggles to pump blood to the lungs. Additionally, heart failure can be acute, developing suddenly, or chronic, gradually worsening over time.
Importance of Diet in Managing Heart Failure
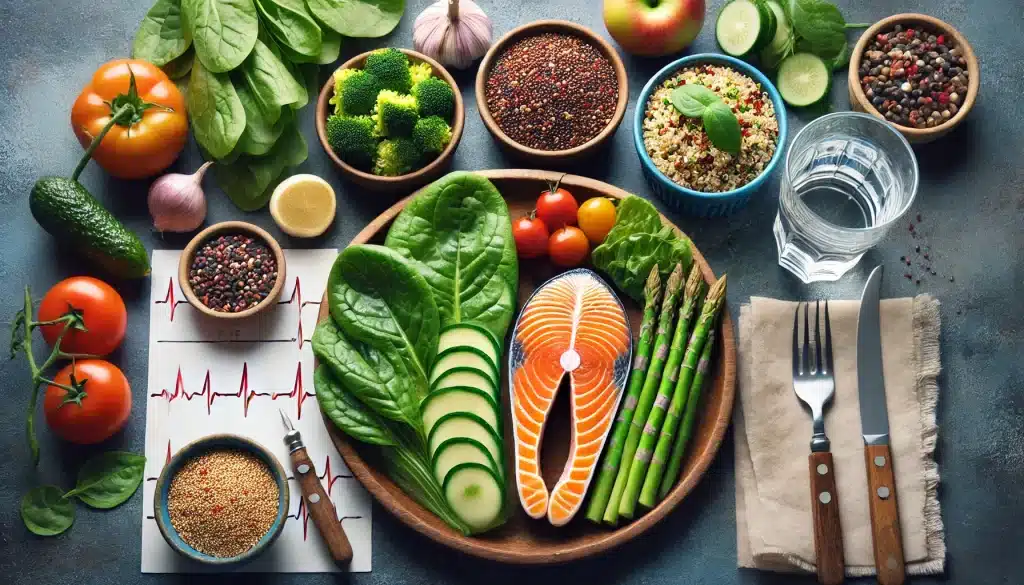
Diet plays a critical role in managing heart failure and preventing further complications. A heart-healthy diet can help reduce the strain on the heart, lower blood pressure, and improve overall cardiovascular function. Patients with heart failure are often advised to follow a balanced, low-sodium, and nutrient-rich diet to support heart health and manage symptoms.
Reducing sodium intake is especially important for heart failure patients, as excess sodium can cause fluid retention, leading to increased stress on the heart and exacerbating symptoms like swelling and shortness of breath. A low-sodium diet helps prevent fluid buildup and supports better heart function.
Incorporating healthy fats, lean proteins, and whole grains into the diet can also contribute to better heart health. A diet rich in fruits and vegetables provides essential vitamins, minerals, and antioxidants that protect against inflammation and oxidative stress, which are common in heart failure patients.
Nutrients That Support Heart Health
Certain nutrients have been shown to support heart health and are particularly beneficial for patients with heart failure. These include:
- Potassium: Helps regulate blood pressure and balance sodium levels in the body. Potassium-rich foods include bananas, sweet potatoes, spinach, and avocados.
- Omega-3 Fatty Acids: Found in fatty fish like salmon, these healthy fats help reduce inflammation and improve cardiovascular health.
- Magnesium: Plays a role in heart rhythm regulation and can be found in foods like nuts, seeds, and leafy green vegetables.
- Fiber: A diet high in fiber helps reduce cholesterol levels and supports overall cardiovascular health. Whole grains, legumes, fruits, and vegetables are excellent sources of fiber.
Foods to Avoid for Heart Failure Patients
For individuals managing heart failure, avoiding certain foods is just as important as incorporating heart-healthy options. These foods can increase the risk of worsening symptoms and lead to complications. Key foods to avoid include:
- High-Sodium Foods: Processed foods, canned soups, salty snacks, and fast food are often high in sodium and should be limited or avoided.
- Sugary Beverages: Sugary drinks like sodas and energy drinks can lead to weight gain and worsen heart failure symptoms.
- Alcohol: Excessive alcohol consumption can weaken the heart muscle and increase the risk of arrhythmias.
- Fried and Fatty Foods: These foods can increase cholesterol levels and contribute to atherosclerosis, which worsens heart failure.
Role of Exercise in Heart Failure Management
Exercise is an essential component in managing heart failure, as it helps improve cardiovascular strength, enhance blood circulation, and reduce the symptoms associated with the condition. Regular physical activity, when done safely, can boost energy levels, improve mood, and even enhance the heart’s ability to pump blood more efficiently. However, for heart failure patients, it’s important to follow a structured and supervised exercise plan to ensure safety.

Studies have shown that patients who engage in regular, moderate exercise often experience an improvement in their overall quality of life. Exercise can help strengthen the heart and reduce the risks associated with heart failure, such as fluid buildup and fatigue. Exercise also promotes healthy weight management, which is crucial for minimizing stress on the heart.
Safe Exercises for Heart Failure Patients
For individuals with heart failure, not all types of exercise are safe. The focus should be on low-impact, moderate-intensity activities that are easy on the joints and do not put too much strain on the heart. Some of the recommended exercises include:
- Walking: Walking is a simple, low-impact exercise that helps improve circulation and cardiovascular strength. Patients should start with short walks and gradually increase the duration.
- Swimming: Water-based exercises are gentle on the joints and allow the body to move more freely while still providing cardiovascular benefits.
- Cycling: Stationary cycling at a moderate pace can be a great way to increase heart rate without overexertion.
- Stretching and Flexibility Exercises: Stretching helps improve flexibility and reduces the risk of injury. Yoga and tai chi are good options for improving flexibility and reducing stress.
It is important for heart failure patients to consult their healthcare provider before starting any exercise program. Monitoring intensity and taking breaks when needed is crucial to avoid overexertion.
Benefits of Regular Physical Activity
The benefits of exercise for heart failure patients extend beyond improved cardiovascular health. Regular physical activity can lead to the following additional benefits:
- Improved Oxygen Use: Exercise helps the body use oxygen more efficiently, reducing the amount of work the heart has to do during physical activity.
- Lower Blood Pressure: Regular activity helps lower blood pressure, reducing strain on the heart and preventing complications related to heart failure.
- Weight Control: Maintaining a healthy weight reduces the overall workload on the heart, which can be particularly beneficial for heart failure patients.
- Better Mental Health: Exercise releases endorphins, which help improve mood, reduce anxiety, and lower stress levels, all of which can improve quality of life for heart failure patients.
Creating a Balanced Plan: Combining Diet and Exercise
To effectively manage heart failure, combining a heart-healthy diet with a regular exercise routine is crucial. Diet and exercise work together to support overall cardiovascular health, reduce symptoms, and improve the patient’s quality of life. A personalized approach that considers the patient’s unique needs, health status, and preferences will ensure long-term success in managing heart failure.

Patients with heart failure should work closely with their healthcare providers to develop a comprehensive plan that incorporates both dietary changes and physical activity. This plan should be tailored to the individual’s condition, including any other underlying health issues such as diabetes or hypertension.
Consistency is key when it comes to diet and exercise in heart failure management. Small, manageable changes over time can have a significant impact on heart health. By setting realistic goals and tracking progress, patients can stay motivated and maintain their routines in the long term.
Personalized Care Plans
Each patient with heart failure has different needs, and what works for one person may not be suitable for another. Personalized care plans are essential to ensure that both diet and exercise programs are aligned with the patient’s overall health status. Factors that should be considered when creating a care plan include:
- Stage of Heart Failure: The severity of heart failure will influence the intensity and type of exercise, as well as specific dietary restrictions.
- Comorbid Conditions: Patients with conditions such as diabetes, hypertension, or kidney disease may require specific dietary adjustments or exercise modifications.
- Physical Abilities: The patient’s physical fitness level will dictate how much activity they can safely engage in, and their diet may need to be adjusted accordingly.
- Medications: Some heart failure medications can interact with certain foods or affect how the body responds to exercise, so these factors must be taken into account.
By focusing on a personalized care plan, patients can achieve the best possible outcomes, improve their quality of life, and manage their symptoms effectively.
Conclusion
Managing heart failure effectively requires a comprehensive approach that includes both dietary changes and regular exercise. A heart-healthy diet helps reduce the strain on the heart by controlling blood pressure, cholesterol levels, and fluid retention, while regular physical activity strengthens the heart muscle and improves overall cardiovascular function. Together, these lifestyle modifications can significantly improve the quality of life for heart failure patients and reduce the risk of complications.
However, it is essential to remember that every patient is unique, and their treatment plans should be tailored to their individual needs. Working closely with healthcare professionals to create a personalized care plan that combines diet, exercise, and medical treatments is crucial for long-term success in managing heart failure. With consistency, patients can achieve better health outcomes and enjoy an improved quality of life.
Incorporating small, sustainable changes to both diet and exercise routines can yield significant improvements over time. By focusing on nutrient-dense foods, avoiding harmful dietary choices, and engaging in safe, regular physical activity, heart failure patients can take control of their condition and enhance their overall well-being.
FAQ
What types of exercises are safe for heart failure patients?
Heart failure patients should focus on low-impact, moderate-intensity exercises such as walking, swimming, and cycling. Stretching and flexibility exercises, like yoga or tai chi, can also be beneficial. It is important to consult a healthcare provider before starting any exercise routine to ensure safety.
How does a low-sodium diet help with heart failure?
A low-sodium diet helps reduce fluid retention, which can ease the workload on the heart. Sodium causes the body to retain water, which can lead to swelling and increased pressure on the heart, worsening heart failure symptoms.
Can heart failure patients eat fatty foods?
Heart failure patients should avoid fried and fatty foods as they can raise cholesterol levels and contribute to the development of atherosclerosis. A heart-healthy diet focuses on lean proteins, healthy fats like those found in fish, and plenty of fruits and vegetables.
How often should heart failure patients exercise?
Patients should aim for regular, moderate-intensity physical activity most days of the week. However, the frequency and duration should be tailored to the individual’s condition and guided by their healthcare provider.
What should heart failure patients avoid in their diet?
Patients should avoid high-sodium foods, sugary beverages, alcohol, and foods high in unhealthy fats. These can worsen symptoms and contribute to other heart-related complications.