Understanding Coronary Artery Disease
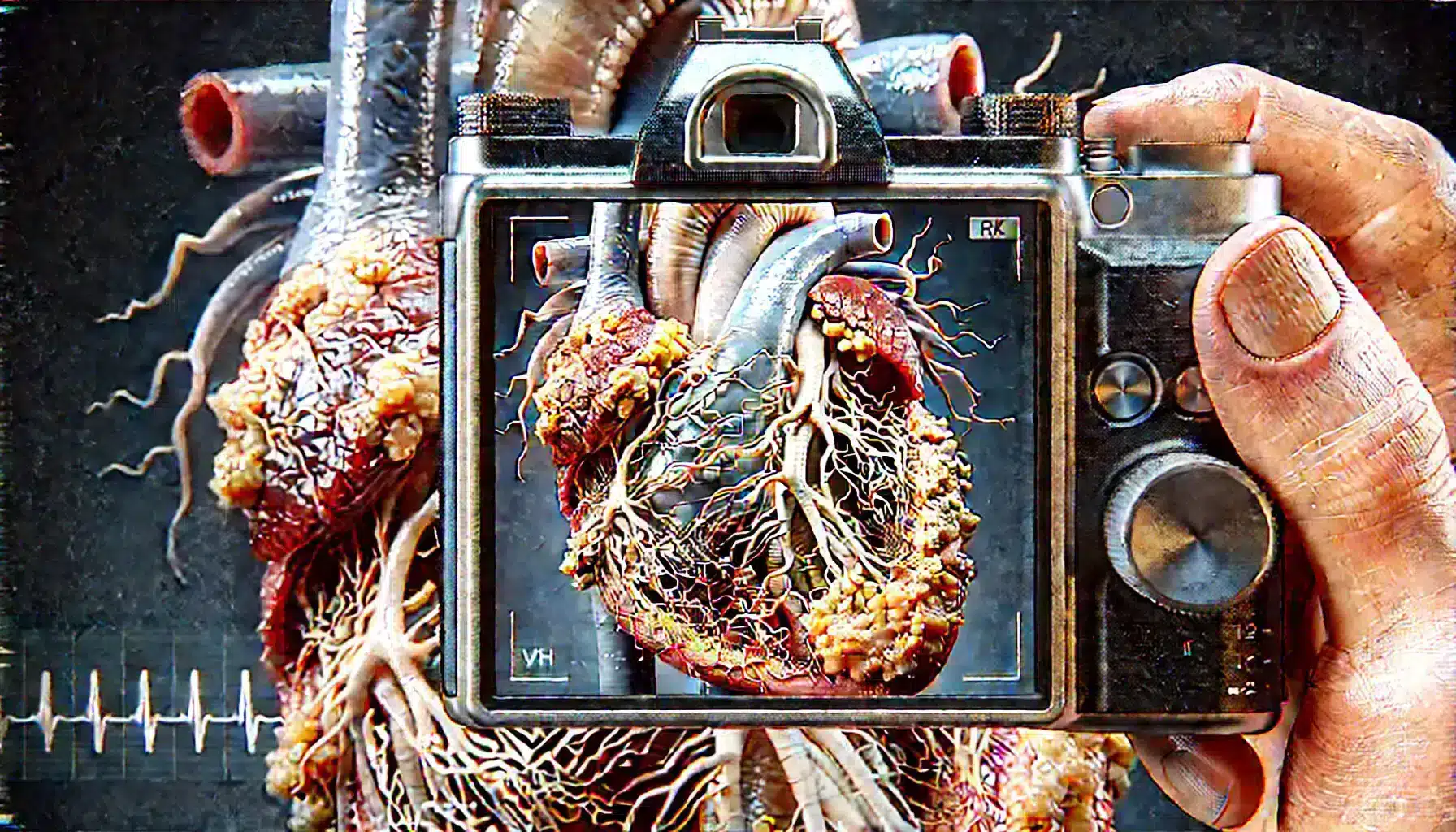
Coronary artery disease (CAD) is a condition characterized by the narrowing or blockage of the coronary arteries, primarily due to atherosclerosis—a buildup of fatty deposits, cholesterol, and other substances on the artery walls. This condition limits the flow of oxygen-rich blood to the heart muscle, which can lead to symptoms like chest pain (angina), shortness of breath, or even heart attacks. Understanding the nature and progression of CAD is crucial for managing the disease and reducing the risk of severe cardiovascular events.
CAD is one of the leading causes of death worldwide. The risk factors include high blood pressure, high cholesterol, smoking, diabetes, obesity, physical inactivity, and a family history of heart disease. While lifestyle changes, medications, and sometimes surgical interventions are used to manage CAD, incorporating a structured exercise program is a key component of treatment. Exercise can improve heart function, reduce symptoms, and enhance overall quality of life for patients with coronary artery disease.
Importance of Exercise for Coronary Artery Disease
Exercise plays a vital role in the management of coronary artery disease. Regular physical activity can help improve cardiovascular health by enhancing blood flow, reducing blood pressure, and increasing the efficiency of the heart muscle. Exercise also helps to control weight, lower LDL (bad) cholesterol levels, raise HDL (good) cholesterol levels, and improve the body’s ability to use insulin, which is particularly important for patients with diabetes or those at risk for it.
In addition to its physical benefits, exercise has been shown to reduce stress, improve mental health, and increase energy levels, all of which can contribute to better heart health. For patients with coronary artery disease, structured exercise programs can significantly decrease the risk of recurrent cardiac events and improve survival rates. However, it’s crucial that the exercise regimen is tailored to the individual’s health status, capabilities, and preferences to maximize benefits while minimizing risks.
General Exercise Recommendations
For patients with coronary artery disease, exercise recommendations should be tailored to individual needs, taking into account the severity of the condition, other existing health issues, and overall fitness levels. The American Heart Association (AHA) and other major health organizations recommend at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, cycling, or swimming. This can be broken down into 30-minute sessions, five days a week, making it more manageable for most individuals.
In addition to aerobic exercise, incorporating strength training at least two days a week can help build muscle mass, improve metabolism, and support overall cardiovascular health. Stretching and flexibility exercises, such as yoga or tai chi, can also be beneficial for improving joint mobility, reducing stress, and enhancing balance. It’s important for patients to start slowly and gradually increase the intensity and duration of exercise as their fitness improves, always listening to their bodies and stopping if they experience any symptoms such as chest pain, dizziness, or severe shortness of breath.

Types of Exercise Suitable for Coronary Artery Disease Patients
Aerobic Exercises
Aerobic exercises are activities that increase the heart rate and improve the efficiency of the cardiovascular system. For coronary artery disease patients, low-to-moderate intensity aerobic exercises are recommended, as they are safe and effective in improving heart health. Examples include brisk walking, cycling, swimming, and light jogging. These activities help to improve oxygen delivery to the heart, reduce blood pressure, and promote better blood sugar control.
It’s advised that patients start with shorter sessions, around 10 to 15 minutes, and gradually increase the duration to reach the recommended 30 minutes per session. Monitoring intensity through the ‘talk test’—being able to maintain a conversation while exercising—can help ensure the activity level is appropriate. Patients should avoid overexertion and should immediately stop exercising if they experience any warning signs such as chest pain or extreme fatigue.
Resistance Training
Resistance training, also known as strength training, involves exercises that improve muscle strength and endurance. For coronary artery disease patients, incorporating resistance training into their routine can help improve overall muscle tone, bone density, and metabolic rate, which supports weight management and heart health. Activities can include the use of free weights, resistance bands, or body-weight exercises like squats and push-ups.
Resistance training should be performed at a moderate intensity, typically with 1-2 sets of 10-15 repetitions of each exercise, targeting all major muscle groups. It is important to start with lighter weights and gradually increase as strength improves, while maintaining proper form to avoid injury. Patients should focus on breathing correctly during exercises, exhaling on exertion, and avoid holding their breath to prevent unnecessary strain on the heart.
Flexibility and Balance Exercises
Flexibility and balance exercises are essential components of a comprehensive exercise program for coronary artery disease patients. Activities like stretching, yoga, and tai chi can help improve the range of motion, reduce muscle stiffness, and enhance overall mobility. These exercises also play a critical role in stress reduction, which is beneficial for heart health. Flexibility exercises can be incorporated into the warm-up and cool-down phases of aerobic and resistance training sessions.
Balance exercises are particularly important for older adults and those at risk of falls. Simple balance activities, such as standing on one leg or walking heel-to-toe, can improve stability and coordination. These exercises should be performed in a safe environment, preferably with support or supervision, especially in the early stages of an exercise program.
Precautions Before Starting an Exercise Program
Before starting an exercise program, it is essential for coronary artery disease patients to consult with their healthcare provider. A thorough medical evaluation, including a stress test or an exercise tolerance test, can help determine the safety and appropriate level of exercise intensity. Based on the results, a tailored exercise plan can be developed that addresses the specific needs and limitations of the patient.
Patients should be aware of the warning signs that may indicate their exercise intensity is too high. Symptoms such as chest pain, unusual shortness of breath, dizziness, palpitations, or excessive fatigue should be taken seriously, and exercise should be stopped immediately. It is also recommended to avoid exercising in extreme weather conditions, such as very hot or cold environments, which can place additional stress on the heart.
For those who are starting a new exercise routine, it’s important to begin gradually, focusing on consistency rather than intensity. Warm-up and cool-down periods are crucial to help the body adjust to the physical activity and reduce the risk of injury. Staying hydrated and wearing appropriate clothing and footwear can further enhance the safety and effectiveness of the exercise program.

Creating a Personalized Exercise Plan
A personalized exercise plan should take into account the individual’s medical history, fitness level, and personal goals. Working with a cardiac rehabilitation specialist or a certified personal trainer who has experience with coronary artery disease patients can be particularly beneficial. The plan should include a balanced mix of aerobic, resistance, and flexibility exercises tailored to the patient’s capabilities and preferences.
Goals should be realistic and achievable, focusing on gradual improvements rather than perfection. For example, the initial goal might be to complete a 10-minute walk daily, with incremental increases in duration and intensity as endurance builds. Tracking progress through a journal or mobile app can help maintain motivation and provide valuable insights into the patient’s progress and any necessary adjustments to the plan.
Patients should also consider incorporating lifestyle changes that complement their exercise routines, such as healthy eating, stress management techniques, and smoking cessation. These changes can have a synergistic effect on improving heart health and overall well-being. Regular follow-ups with healthcare providers can ensure the exercise plan remains aligned with the patient’s evolving health needs and goals.
Monitoring Progress and Adjusting the Plan
Monitoring progress is a critical aspect of any exercise program for coronary artery disease patients. Regular check-ins with healthcare providers, such as cardiologists or exercise physiologists, can help assess how well the exercise plan is working and make necessary adjustments. Patients should keep track of their exercise routines, including the type, duration, and intensity of activities, as well as any symptoms experienced during or after exercise.
Using wearable devices like heart rate monitors or fitness trackers can provide valuable feedback on exercise intensity and overall activity levels. These tools can help patients stay within their recommended heart rate zones, ensuring that exercise remains safe and effective. Additionally, tracking improvements in fitness, such as increased endurance or strength, can be encouraging and motivate patients to stick with their exercise routines.
Adjustments to the exercise plan may be needed based on progress, new medical conditions, or changes in symptoms. For instance, if a patient finds that they can comfortably complete their current exercise regimen, the plan might be adjusted to increase the intensity or duration. Conversely, if new symptoms arise or existing ones worsen, a temporary reduction in activity levels or a shift to lower-intensity exercises may be necessary. Ongoing communication with healthcare providers is essential to ensure the exercise plan remains aligned with the patient’s health status and goals.
General Exercise Recommendations
For patients with coronary artery disease, exercise recommendations should be tailored to individual needs, taking into account the severity of the condition, other existing health issues, and overall fitness levels. Here are some general guidelines:
- Aerobic Exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, cycling, or swimming. This can be broken into 30-minute sessions, five days a week.
- Strength Training: Include resistance training at least two days a week, focusing on major muscle groups to improve muscle mass and metabolism.
- Flexibility and Balance: Incorporate flexibility and balance exercises like stretching, yoga, or tai chi to enhance mobility and reduce stress.
- Start Slow: Begin with short sessions and gradually increase the duration and intensity as fitness improves.
- Listen to Your Body: Stop exercising immediately if you experience symptoms like chest pain, dizziness, or severe shortness of breath.
Frequently Asked Questions
What types of exercises are best for coronary artery disease patients?
Coronary artery disease patients benefit most from aerobic exercises such as walking, cycling, and swimming, combined with resistance training and flexibility exercises. It’s important to start slowly and gradually increase intensity, with the guidance of healthcare providers.
Can exercise reduce the risk of heart attacks for coronary artery disease patients?
Yes, regular exercise can significantly reduce the risk of heart attacks in coronary artery disease patients by improving cardiovascular function, lowering blood pressure, reducing cholesterol levels, and helping to maintain a healthy weight.
Are there any exercises that coronary artery disease patients should avoid?
Patients should avoid high-intensity exercises that may strain the heart excessively, such as heavy weightlifting or intense interval training, without proper medical clearance. It’s also advised to avoid exercising in extreme temperatures and to always warm up before starting.
How can I know if my exercise intensity is appropriate?
The “talk test” is a simple way to gauge exercise intensity: if you can carry on a conversation while exercising, the intensity is likely appropriate. Using heart rate monitors or checking perceived exertion levels can also help ensure exercise remains safe.
How often should coronary artery disease patients exercise?
Patients are generally advised to engage in at least 150 minutes of moderate-intensity aerobic exercise per week, spread across most days of the week, combined with strength training on at least two days. Flexibility and balance exercises can be added to support overall fitness and heart health.