What is Sleep Apnea?
Sleep apnea is a common but serious sleep disorder where breathing repeatedly stops and starts during sleep. This condition can lead to poor sleep quality and various health issues if left untreated. There are two main types of sleep apnea: obstructive sleep apnea (OSA), which occurs when the throat muscles relax and block the airway, and central sleep apnea (CSA), which happens when the brain fails to send proper signals to the muscles that control breathing.

In obstructive sleep apnea, the airway becomes physically blocked, often due to soft tissue in the throat collapsing. Central sleep apnea, on the other hand, involves a failure of the central nervous system to initiate breathing, making it a more complex form of the condition. Both forms of sleep apnea can severely impact a person’s quality of life and overall health.
- Obstructive Sleep Apnea (OSA)
- Central Sleep Apnea (CSA)
Although people may not always realize they have sleep apnea, its symptoms are often noticeable to those who share the same sleeping space. Common signs include loud snoring, episodes of breathing cessation during sleep, gasping for air, excessive daytime sleepiness, and morning headaches.
How Does Sleep Apnea Affect the Heart?
Sleep apnea doesn’t just disrupt sleep; it has a profound impact on the cardiovascular system, particularly the heart. Every time a person with sleep apnea experiences a pause in breathing, oxygen levels in the blood drop significantly. This condition, called hypoxia, puts the body under stress, forcing the heart to work harder to pump blood and compensate for the lack of oxygen. Over time, this strain can lead to a variety of heart-related problems, including high blood pressure, heart failure, and arrhythmias.
During an apneic event, the body triggers a “fight or flight” response, releasing stress hormones like adrenaline. This not only raises blood pressure but also makes the heart rhythm more susceptible to disturbances. In fact, people with sleep apnea are at a significantly higher risk of developing heart arrhythmias—irregular heartbeats that can be life-threatening if left unmanaged.
- Increased stress on the heart due to oxygen deprivation
- Release of stress hormones, raising blood pressure
- Higher risk of heart-related issues, including arrhythmias
The chronic, repeated nature of these breathing interruptions places immense pressure on the heart, which over time can result in long-term cardiovascular complications. Studies show that untreated sleep apnea is linked to a higher incidence of heart attacks, stroke, and sudden cardiac death.
Understanding Heart Arrhythmias
Heart arrhythmias are conditions where the heart beats irregularly, too fast (tachycardia), or too slow (bradycardia). Normally, the heart beats in a regular rhythm controlled by electrical signals that trigger the heart’s chambers to contract and pump blood. When these signals are disrupted, an arrhythmia can occur, leading to irregular heartbeats that may feel like fluttering, racing, or slowing down of the heart.
Arrhythmias are classified based on where they originate in the heart. Supraventricular arrhythmias occur in the atria, the upper chambers of the heart, while ventricular arrhythmias occur in the ventricles, the heart’s lower chambers. These conditions range from harmless to life-threatening, depending on the type, frequency, and underlying cause.
- Supraventricular arrhythmias: Occur in the upper chambers (atria) of the heart
- Ventricular arrhythmias: Occur in the lower chambers (ventricles) of the heart
Some common symptoms of arrhythmias include palpitations, dizziness, shortness of breath, chest pain, and in severe cases, fainting or collapse. It is crucial to identify and manage arrhythmias early, as they can lead to more severe complications like stroke or heart failure if untreated.
The Link Between Sleep Apnea and Heart Arrhythmias
The connection between sleep apnea and heart arrhythmias is well-established in medical literature. When sleep apnea causes intermittent pauses in breathing, the body’s oxygen levels decrease dramatically. This oxygen deprivation (hypoxia) triggers a cascade of physiological responses, including an increase in sympathetic nervous system activity, which releases stress hormones like adrenaline. These responses not only raise blood pressure but also increase the likelihood of developing arrhythmias.
Research has shown that people with obstructive sleep apnea (OSA) have a significantly higher risk of developing atrial fibrillation (AFib), one of the most common forms of arrhythmia. Sleep apnea-induced hypoxia also leads to structural changes in the heart over time, such as enlargement of the left atrium, which is another risk factor for AFib and other arrhythmias.
- Oxygen deprivation leads to stress on the heart
- Increased risk of developing atrial fibrillation and other arrhythmias
- Long-term structural changes in the heart due to sleep apnea
The link between sleep apnea and heart arrhythmias highlights the importance of diagnosing and treating sleep apnea in patients who are at risk for or already have cardiovascular disease. Early intervention with treatments such as CPAP (Continuous Positive Airway Pressure) therapy can reduce the occurrence of arrhythmias and improve heart health outcomes.
Physiological Mechanisms of Sleep Apnea on Heart Rhythms
Several physiological mechanisms explain how sleep apnea can trigger heart arrhythmias. First, repeated apneic events cause fluctuations in intrathoracic pressure, which can stretch and stress the heart muscle, particularly the atria. This mechanical stress, combined with hypoxia, can lead to electrical instability in the heart’s conduction system, making arrhythmias more likely.
Additionally, during apneic episodes, the body experiences episodes of hypoxia followed by reoxygenation, creating oxidative stress. This oxidative stress damages blood vessels and cardiac tissue, increasing the risk of arrhythmias. Furthermore, the activation of the sympathetic nervous system during apneic events raises heart rate and blood pressure, further contributing to arrhythmia risk.
Role of Oxygen Deprivation in Arrhythmia Risk
Oxygen deprivation, or hypoxia, plays a critical role in the development of arrhythmias in people with sleep apnea. During an apnea event, the body receives less oxygen, which forces the heart to work harder to pump oxygenated blood throughout the body. Hypoxia triggers a response from the autonomic nervous system, particularly the sympathetic nervous system, which releases adrenaline and other stress hormones that stimulate the heart. This can lead to irregular heartbeats and increases the overall risk of arrhythmias.
Moreover, chronic oxygen deprivation over time can lead to permanent changes in heart tissue, such as scarring and fibrosis, which further increases the likelihood of arrhythmias. This is particularly evident in patients with obstructive sleep apnea, where repeated cycles of low oxygen and high stress eventually damage the heart’s electrical system, leading to both atrial and ventricular arrhythmias.
- Hypoxia triggers sympathetic nervous system activation
- Chronic oxygen deprivation leads to heart tissue damage
- Increased risk of atrial and ventricular arrhythmias
Research Studies on Sleep Apnea and Arrhythmias
Numerous studies have demonstrated the strong association between sleep apnea and arrhythmias. One large-scale study published in the *Journal of the American College of Cardiology* found that patients with obstructive sleep apnea had a 2-4 times higher risk of developing atrial fibrillation compared to those without sleep apnea. Another study highlighted the fact that treating sleep apnea with CPAP therapy significantly reduced the incidence of arrhythmias, emphasizing the importance of early diagnosis and treatment.
Research also indicates that the severity of sleep apnea correlates with the risk of arrhythmias. Those with moderate to severe obstructive sleep apnea are more likely to develop complex arrhythmias, including life-threatening ventricular arrhythmias. These findings underscore the need for comprehensive screening in patients with sleep apnea, especially those with existing cardiovascular conditions.
Common Types of Arrhythmias Associated with Sleep Apnea
There are several types of heart arrhythmias that are commonly associated with sleep apnea. These irregular heartbeats can range from mild to severe and are often worsened by the physiological effects of oxygen deprivation and increased cardiac strain caused by sleep apnea. Understanding the types of arrhythmias linked to sleep apnea is crucial for early diagnosis and treatment.
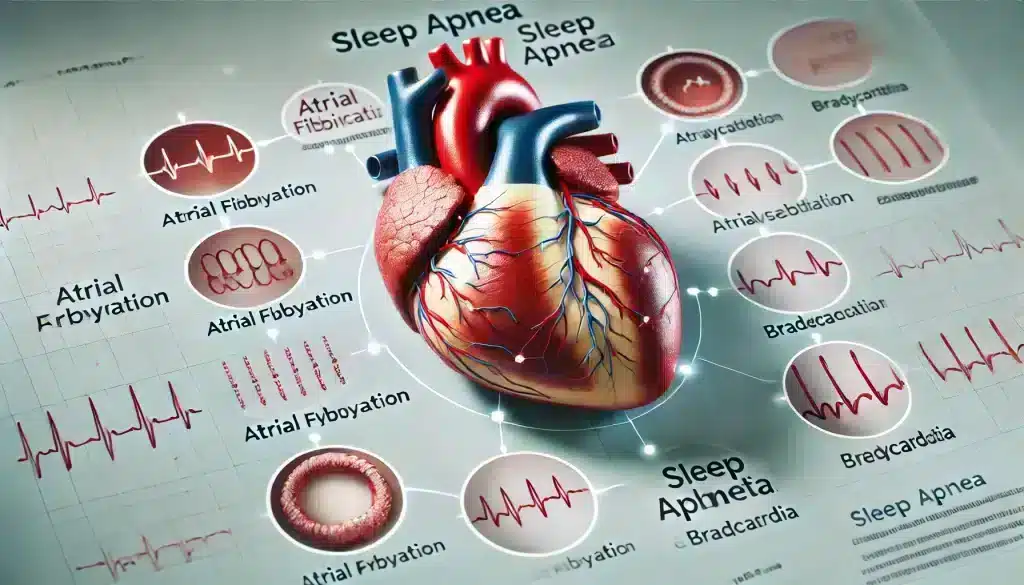
Atrial Fibrillation and Sleep Apnea
Atrial fibrillation (AFib) is the most common arrhythmia associated with sleep apnea. AFib occurs when the electrical signals in the atria, the heart’s upper chambers, become disorganized, causing the heart to beat irregularly and often rapidly. Studies have shown that people with sleep apnea are significantly more likely to develop AFib compared to the general population, especially if their sleep apnea is untreated.
AFib can cause a wide range of symptoms, including palpitations, shortness of breath, dizziness, and fatigue. More importantly, AFib can lead to serious complications such as stroke and heart failure. Treating sleep apnea has been shown to reduce the frequency and severity of AFib episodes, highlighting the importance of managing both conditions together.
Bradycardia and Sleep Apnea
Bradycardia, or a slow heart rate, is another type of arrhythmia that can occur in people with sleep apnea. During apneic events, the oxygen levels in the blood drop, and the body’s response is to slow down the heart rate in an effort to conserve oxygen. While bradycardia is usually harmless, in severe cases it can lead to dizziness, fainting, or even cardiac arrest if left unmanaged.
The repeated drops in heart rate seen in sleep apnea patients can eventually lead to permanent changes in the heart’s electrical system, making bradycardia more likely to occur. Managing sleep apnea with treatments like CPAP can help stabilize heart rhythms and prevent dangerous episodes of bradycardia.
Ventricular Arrhythmias and Sleep Apnea
Ventricular arrhythmias are irregular heartbeats that originate in the ventricles, the heart’s lower chambers. These arrhythmias can be life-threatening, especially if they lead to ventricular fibrillation, a condition where the heart cannot effectively pump blood. People with sleep apnea, particularly those with severe obstructive sleep apnea, are at a higher risk for developing ventricular arrhythmias due to the stress and strain placed on the heart.
Hypoxia, increased sympathetic nervous system activity, and high blood pressure—all common in sleep apnea—can trigger ventricular arrhythmias. Treating sleep apnea is essential for reducing the risk of these dangerous arrhythmias and improving overall heart health.
Diagnosing Sleep Apnea in Heart Patients
Diagnosing sleep apnea in patients who are at risk of or already have heart conditions is crucial for preventing further cardiovascular complications. Since sleep apnea often goes undiagnosed, particularly in those who do not exhibit classic symptoms like loud snoring, it is essential for healthcare providers to conduct thorough evaluations, especially when heart arrhythmias are present. Early diagnosis can improve treatment outcomes and reduce the risk of developing serious heart issues.

Sleep apnea diagnosis typically involves monitoring a patient’s breathing patterns, heart rate, and oxygen levels during sleep. The most common diagnostic tool for sleep apnea is a sleep study, known as polysomnography, which records various body functions during sleep to identify the presence and severity of the condition. Portable home sleep tests are also available and can provide valuable insights for diagnosing sleep apnea in a more convenient setting.
- Polysomnography (sleep study)
- Home sleep apnea tests
- Monitoring heart rate and oxygen levels
Sleep Studies and Heart Monitoring
During a sleep study, sensors are placed on the patient’s body to monitor brain activity, breathing patterns, oxygen levels, heart rate, and muscle movements. These tests provide a comprehensive overview of how sleep apnea affects the body, particularly the heart. For heart patients, sleep studies often include additional monitoring to track heart rhythms and detect arrhythmias that may occur during apneic events.
Sleep studies are especially important for patients who have been diagnosed with arrhythmias such as atrial fibrillation or ventricular arrhythmias, as sleep apnea can exacerbate these conditions. Continuous monitoring of heart activity during sleep helps healthcare providers identify potential triggers and implement appropriate treatments.
Screening Tools and Techniques
Aside from sleep studies, there are other screening tools and techniques used to diagnose sleep apnea, particularly in patients with cardiovascular conditions. These include questionnaires like the Epworth Sleepiness Scale and the STOP-BANG questionnaire, which assess the risk of sleep apnea based on daytime sleepiness, snoring habits, and other factors.
For heart patients, ambulatory monitoring devices, such as portable ECG monitors, may also be used to detect arrhythmias and assess heart function during sleep. These tools provide valuable data that can guide treatment decisions and help manage both sleep apnea and heart arrhythmias more effectively.
Treatment Approaches for Sleep Apnea to Prevent Arrhythmias
Treating sleep apnea is essential for preventing heart arrhythmias and improving overall cardiovascular health. The primary goal of treatment is to ensure uninterrupted breathing during sleep, which helps maintain normal oxygen levels and reduces the strain on the heart. Effective management of sleep apnea can significantly lower the risk of arrhythmias and improve the quality of life for patients.
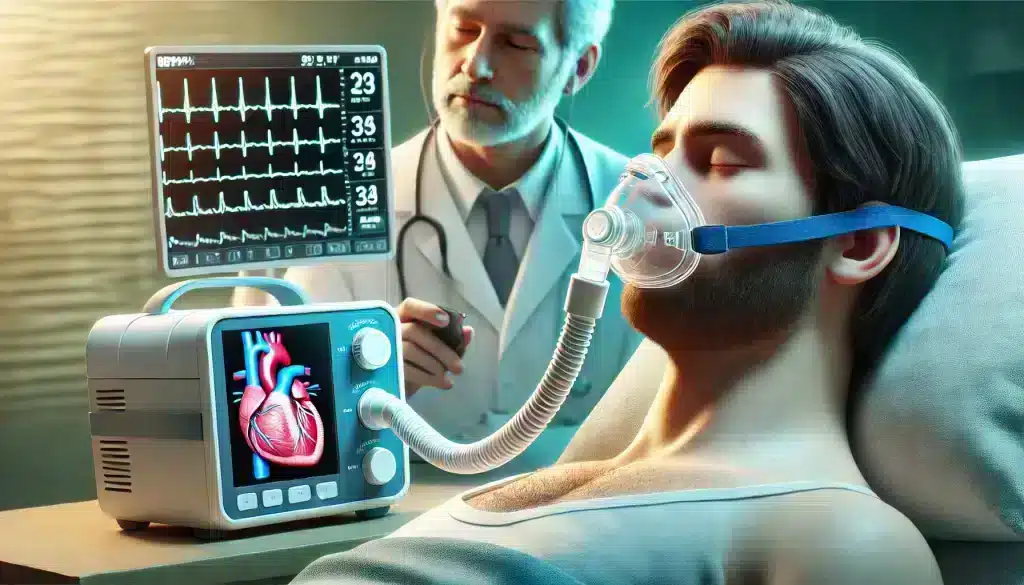
The most common and effective treatment for obstructive sleep apnea is Continuous Positive Airway Pressure (CPAP) therapy, which uses a machine to deliver a steady stream of air to keep the airway open during sleep. However, lifestyle changes and other medical interventions can also play a role in managing sleep apnea and reducing arrhythmia risk.
- CPAP therapy as the first-line treatment
- Lifestyle changes for improved heart health
- Surgical interventions for severe cases
CPAP Therapy for Reducing Arrhythmias
CPAP therapy is the gold standard for treating obstructive sleep apnea. By providing continuous airflow, CPAP prevents the airway from collapsing during sleep, ensuring that oxygen levels remain stable. Studies have shown that patients who use CPAP therapy regularly experience fewer episodes of arrhythmias, particularly atrial fibrillation, as well as improved overall heart function.
In addition to preventing arrhythmias, CPAP therapy also helps lower blood pressure, reduce stress on the heart, and improve sleep quality. For patients with sleep apnea and heart arrhythmias, CPAP can be a life-changing treatment that not only addresses breathing problems but also protects the heart from further damage.
Lifestyle Changes and Arrhythmia Management
In addition to CPAP therapy, certain lifestyle changes can help manage sleep apnea and reduce the risk of arrhythmias. Weight loss is one of the most effective strategies for improving sleep apnea, as excess weight contributes to the narrowing of the airway. Regular physical activity and a heart-healthy diet are also essential for managing both sleep apnea and cardiovascular conditions.
Other lifestyle changes that can benefit patients include quitting smoking, reducing alcohol consumption, and managing stress. These modifications can lower the frequency and severity of sleep apnea episodes, as well as reduce the overall risk of developing arrhythmias.
Frequently Asked Questions (FAQ)
How does sleep apnea increase the risk of heart arrhythmias?
Sleep apnea increases the risk of heart arrhythmias by causing oxygen deprivation (hypoxia) during apneic episodes. This lack of oxygen triggers stress responses in the body, including the release of stress hormones and increased sympathetic nervous system activity, which can lead to irregular heart rhythms. Over time, these repeated episodes of oxygen deprivation can cause structural changes in the heart, further increasing the risk of arrhythmias.
Can treating sleep apnea help prevent arrhythmias?
Yes, treating sleep apnea can significantly reduce the risk of developing arrhythmias. Continuous Positive Airway Pressure (CPAP) therapy, which keeps the airway open during sleep, is the most effective treatment for obstructive sleep apnea. By ensuring proper oxygenation and reducing the strain on the heart, CPAP therapy can lower the incidence of arrhythmias and improve overall heart health.
What types of arrhythmias are most commonly associated with sleep apnea?
The most common arrhythmias associated with sleep apnea are atrial fibrillation (AFib), bradycardia (slow heart rate), and ventricular arrhythmias. AFib, in particular, has a strong link with obstructive sleep apnea, and patients with untreated sleep apnea are at a higher risk of developing this irregular heart rhythm.
What are the symptoms of sleep apnea-related arrhythmias?
Symptoms of arrhythmias in people with sleep apnea may include palpitations (a fluttering or racing heart), dizziness, shortness of breath, chest pain, and in severe cases, fainting or sudden collapse. If these symptoms occur frequently, it’s essential to consult a healthcare provider for proper diagnosis and treatment.
How can I find out if I have sleep apnea?
If you suspect you have sleep apnea, it’s important to consult a healthcare professional for evaluation. A sleep study (polysomnography) is the most common diagnostic tool for identifying sleep apnea. Portable home sleep tests are also available and can provide valuable insights. Common symptoms to look out for include loud snoring, gasping for air during sleep, and excessive daytime sleepiness.
Conclusion
Sleep apnea is a serious condition that not only affects the quality of sleep but also poses significant risks to heart health, particularly in the development of heart arrhythmias. The intermittent oxygen deprivation that occurs during apneic episodes places immense stress on the cardiovascular system, triggering irregular heart rhythms like atrial fibrillation, bradycardia, and ventricular arrhythmias. If left untreated, sleep apnea can lead to long-term damage to the heart and increase the risk of complications such as stroke, heart failure, and sudden cardiac death.
Fortunately, sleep apnea can be effectively managed with treatments such as CPAP therapy, which has been shown to reduce the occurrence of arrhythmias and improve overall heart function. Additionally, lifestyle changes such as weight loss, quitting smoking, and adopting a heart-healthy diet can further reduce the severity of sleep apnea and lower the risk of arrhythmias. Early diagnosis and treatment are essential for preventing the potentially life-threatening consequences of sleep apnea and protecting heart health.
If you suspect that you or a loved one may have sleep apnea, it is important to seek medical attention and undergo proper evaluation. By addressing sleep apnea early and implementing the appropriate treatments, you can safeguard your heart and improve your overall quality of life.



