What is Coronary Angiography?
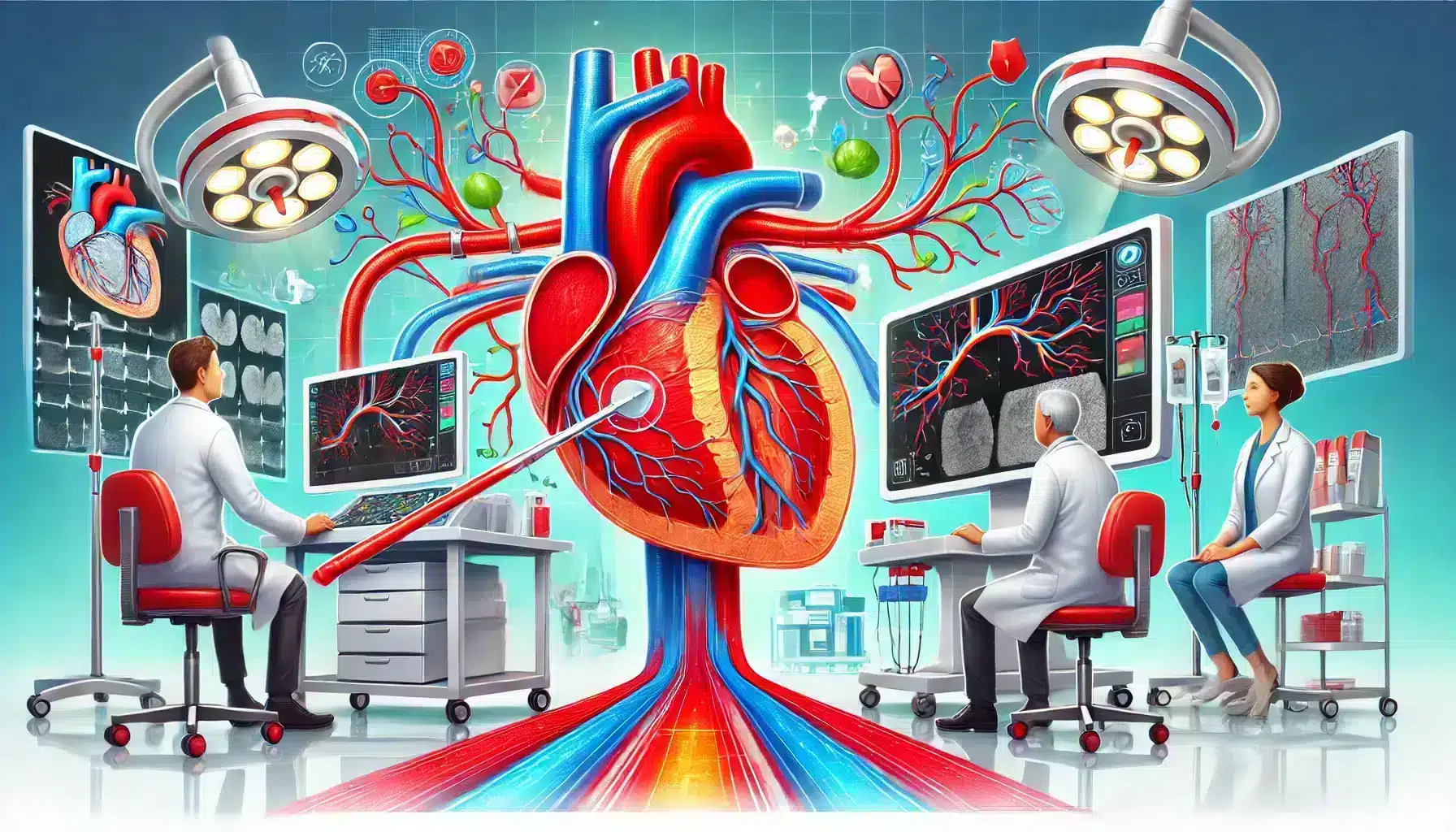
Coronary angiography is a specialized medical imaging procedure used to visualize the coronary arteries, which supply blood to the heart muscle. This diagnostic test allows doctors to assess the presence and severity of blockages or narrowing within these arteries, which could lead to serious heart conditions such as coronary artery disease or heart attacks. By injecting a contrast dye into the bloodstream and using X-ray technology, the procedure provides detailed images of the heart’s blood vessels, enabling doctors to evaluate the heart’s blood flow and identify any obstructions.
Angiography is a vital tool in modern cardiology, particularly for patients experiencing chest pain, shortness of breath, or other symptoms indicative of heart disease. It is often performed to diagnose conditions like coronary artery disease or to determine the best treatment options for individuals with known heart problems. In some cases, coronary angiography may also be used as a guide during interventional procedures, such as stent placement or angioplasty, to restore normal blood flow in blocked arteries.
- Provides detailed images of the coronary arteries
- Helps diagnose conditions like coronary artery disease and blockages
- Can guide interventional procedures like stent placement or angioplasty
For patients with known risk factors for heart disease, such as high cholesterol, high blood pressure, smoking, or a family history of heart problems, coronary angiography can be an essential diagnostic tool. Early detection of blockages or arterial narrowing allows for timely intervention, reducing the risk of more severe complications, such as heart attacks or heart failure. Understanding what this procedure entails and its importance in heart disease diagnosis can help patients and doctors make informed decisions about treatment.
Why is Coronary Angiography Performed?
Coronary angiography is primarily performed to investigate symptoms of heart disease, such as chest pain (angina), shortness of breath, dizziness, or fatigue. These symptoms often indicate that blood flow to the heart is restricted due to blockages or narrowing in the coronary arteries. By conducting an angiogram, doctors can pinpoint the exact location and severity of these blockages, allowing them to make precise diagnoses and recommend appropriate treatments, such as medication, lifestyle changes, or surgical interventions like angioplasty or bypass surgery.
In addition to diagnosing symptomatic patients, coronary angiography is also used to assess heart health in individuals who may be at risk for heart disease but have not yet shown symptoms. For example, patients with high cholesterol, high blood pressure, or a strong family history of heart disease may undergo angiography as a precautionary measure. This proactive approach helps detect early-stage coronary artery disease, preventing it from progressing to more dangerous conditions, such as a heart attack.
Common Reasons for Coronary Angiography
There are several common scenarios where doctors recommend a coronary angiogram:
- **Chest Pain or Angina:** Persistent chest pain that does not improve with medication or rest may indicate a blockage in the coronary arteries. A coronary angiogram can help identify the source of the blockage and guide treatment.
- **Abnormal Stress Test Results:** If a patient shows abnormal results during a stress test (which measures how the heart performs under physical exertion), a coronary angiogram may be ordered to visualize the arteries more clearly.
- **Shortness of Breath:** Difficulty breathing can be a sign of heart disease, especially if the patient has other risk factors, such as diabetes, high cholesterol, or a history of smoking.
- **Unstable Angina or Heart Attack:** In emergency situations, such as an ongoing heart attack or episodes of unstable angina, a coronary angiogram is often used to quickly assess and treat blocked arteries.
- **Pre-surgical Evaluation:** Before procedures like heart valve replacement or bypass surgery, doctors may use an angiogram to evaluate the health of the coronary arteries.
In each of these cases, the goal of the coronary angiography is to gather detailed information about the coronary arteries, allowing doctors to determine the best course of action. It is a critical tool in modern cardiology, enabling precise and personalized care for patients with varying degrees of heart disease.
Diagnosing Coronary Artery Disease
Coronary artery disease (CAD) is one of the most common heart conditions diagnosed using angiography. CAD occurs when the coronary arteries become narrowed or blocked due to a buildup of plaque (atherosclerosis). This buildup restricts blood flow to the heart, leading to chest pain, shortness of breath, or in severe cases, heart attacks. The images produced by a coronary angiogram provide doctors with a clear view of these blockages, helping them diagnose the extent of the disease and plan the necessary treatments.
For patients diagnosed with coronary artery disease, the next steps may involve medication to manage symptoms and slow the progression of plaque buildup, lifestyle changes such as a heart-healthy diet and regular exercise, or more invasive treatments like stent placement or coronary artery bypass surgery. Early detection through angiography can prevent CAD from worsening and improve the patient’s long-term prognosis.
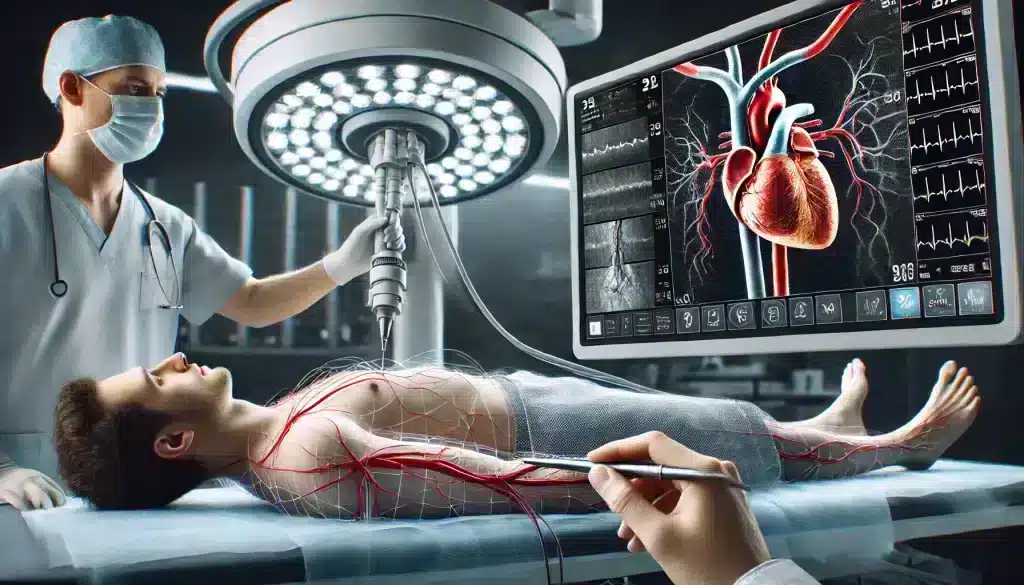
The Coronary Angiography Procedure: Step-by-Step
Understanding how a coronary angiography procedure is performed can help alleviate any concerns or anxiety about undergoing the test. This diagnostic procedure is typically done in a hospital setting or specialized cardiac center by a cardiologist. The procedure is considered minimally invasive, but it does require careful preparation and attention to detail to ensure accurate results and patient safety.
Preparing for the Procedure
Before undergoing a coronary angiogram, patients are advised to follow specific preparation instructions. These may include:
- Fasting: Patients are often asked to fast for several hours before the procedure to ensure that their stomach is empty.
- Medication Adjustments: Some medications, particularly blood thinners, may need to be paused or adjusted before the procedure to reduce the risk of bleeding.
- Allergy Check: Since the procedure involves the injection of a contrast dye, it’s important to check for any allergies to the dye or iodine. Patients should inform their doctor if they’ve experienced allergic reactions in the past.
- Pre-procedure Testing: In some cases, doctors may recommend a blood test or electrocardiogram (ECG) before the angiogram to evaluate the patient’s overall heart health.
Preparing for a coronary angiography also involves discussing any existing medical conditions or recent health issues with the healthcare provider. Proper preparation helps ensure that the procedure goes smoothly and reduces the risk of complications.
What Happens During Coronary Angiography?
On the day of the procedure, the patient will be taken to a catheterization lab, where the coronary angiogram will take place. The patient is typically awake during the procedure but may be given a mild sedative to help them relax. A local anesthetic is applied to numb the area where the catheter will be inserted—usually in the groin or wrist.
Once the area is numbed, the doctor inserts a thin, flexible tube (catheter) into a blood vessel and guides it toward the heart using X-ray imaging. A special contrast dye is then injected through the catheter, allowing the coronary arteries to become visible on an X-ray screen. The doctor carefully observes the flow of blood through the coronary arteries, looking for any blockages or narrowings that may be causing symptoms or increasing the patient’s risk of a heart attack.
- Catheter Insertion: A thin tube is inserted into a blood vessel in the wrist or groin and guided toward the heart.
- Contrast Dye Injection: A contrast dye is injected to highlight the coronary arteries on X-ray images.
- Observation: The doctor watches the blood flow through the coronary arteries, identifying any blockages or narrowing.
The entire procedure usually takes between 30 minutes and an hour, depending on the complexity of the patient’s condition. After the test, the catheter is removed, and pressure is applied to the insertion site to stop any bleeding. Patients are then taken to a recovery area for observation.
Coronary angiography is a relatively safe and quick procedure, but it provides vital information about a patient’s heart health. It allows doctors to make informed decisions about whether treatments like medication, stenting, or bypass surgery are necessary. In some cases, interventional procedures may be performed immediately following the angiogram to restore blood flow in blocked arteries.
Risks and Complications of Coronary Angiography
While coronary angiography is considered a safe and routine procedure, it is still a medical intervention that carries some risks. Understanding the potential risks and complications helps patients make informed decisions about their heart health. Most complications are rare and can be managed effectively with proper care, but it’s important to be aware of them before undergoing the procedure.
Potential Risks to Consider
The risks associated with coronary angiography are generally low, but they can vary depending on the patient’s overall health, age, and the complexity of the procedure. Some potential risks include:
- Allergic Reaction to Contrast Dye: Some patients may experience an allergic reaction to the contrast dye used in the angiogram. This reaction can range from mild itching to more severe symptoms like difficulty breathing or swelling. Patients with a known allergy to iodine or contrast dye should inform their doctor before the procedure.
- Bleeding or Bruising at the Catheter Site: Since a catheter is inserted into a blood vessel, there is a small risk of bleeding or bruising at the insertion site. In some cases, a hematoma (a collection of blood under the skin) may develop.
- Blood Vessel Damage: Although rare, the catheter may cause damage to the blood vessel as it is inserted or maneuvered through the artery.
- Heart Attack or Stroke: In very rare cases, complications during the procedure may lead to a heart attack or stroke, particularly if the patient already has severe heart disease.
- Kidney Damage: The contrast dye used in the procedure can sometimes affect kidney function, especially in patients with pre-existing kidney issues or diabetes.
Most of these risks are uncommon, and doctors take steps to minimize them during the procedure. By discussing these risks beforehand, patients can feel more prepared and confident about undergoing the coronary angiogram.
How Doctors Minimize Risks
To reduce the likelihood of complications, doctors take several precautionary measures during and after the coronary angiography. These include:
- Thorough Pre-procedure Assessment: Before performing the angiogram, doctors evaluate the patient’s medical history, current medications, and any pre-existing conditions, such as allergies or kidney issues, to tailor the procedure and minimize risks.
- Use of Advanced Technology: Modern catheterization labs are equipped with advanced imaging technology that allows doctors to navigate the coronary arteries with precision, reducing the risk of damage to blood vessels.
- Monitoring During the Procedure: Throughout the procedure, the patient’s heart rate, blood pressure, and oxygen levels are closely monitored to detect any signs of complications early.
- Post-procedure Care: After the angiogram, patients are carefully observed in a recovery area. Pressure is applied to the catheter insertion site to prevent bleeding, and patients are advised to rest for several hours to aid in recovery.
By following these precautions, doctors ensure that the coronary angiography is as safe as possible. While the risks are minimal, it’s crucial for patients to have a clear understanding of the procedure and potential complications before proceeding.
Recovery After Coronary Angiography
After undergoing a coronary angiography, recovery is typically quick and straightforward, but it’s important for patients to follow the recommended guidelines to ensure a smooth recovery. Most patients are able to return home the same day, especially if the procedure was performed on an outpatient basis. However, depending on the complexity of the procedure or if additional interventions, such as stent placement, were performed, recovery times may vary slightly.
Immediate Post-Procedure Care
Once the coronary angiogram is complete, patients are taken to a recovery area where they are closely monitored for any signs of complications. Here’s what to expect immediately after the procedure:
- Monitoring and Observation: Vital signs, including heart rate and blood pressure, are monitored to ensure the patient is stable. The insertion site, whether in the wrist or groin, is also checked regularly for any signs of bleeding or swelling.
- Pressure on the Catheter Site: After the catheter is removed, pressure is applied to the insertion site for several minutes to prevent bleeding. In some cases, a special closure device may be used to seal the puncture site.
- Rest and Hydration: Patients are encouraged to rest and stay hydrated to help flush the contrast dye from the body and reduce the risk of kidney issues. Patients may need to lie flat for a few hours, especially if the catheter was inserted through the groin, to ensure proper healing.
Most patients can leave the hospital or clinic a few hours after the procedure if no complications arise. However, some patients may need to stay overnight for observation, especially if additional procedures were performed during the angiogram.
Long-Term Recovery and Follow-Up
While the immediate recovery from a coronary angiography is typically quick, patients should follow specific guidelines during the longer recovery period. These include:
- Avoiding Strenuous Activity: Patients should avoid heavy lifting, strenuous exercise, or any activity that puts pressure on the insertion site for at least a week to allow it to heal fully.
- Medication Adherence: Depending on the angiogram results, doctors may prescribe medications, such as blood thinners or cholesterol-lowering drugs, to reduce the risk of future heart problems. Patients must follow their medication plan as prescribed.
- Follow-up Appointments: It is important to attend all follow-up appointments with the cardiologist to review the angiogram results, discuss next steps, and monitor ongoing heart health.
- Watch for Warning Signs: Patients should be aware of any unusual symptoms, such as excessive swelling or bleeding at the catheter site, shortness of breath, or chest pain, and contact their doctor immediately if these occur.
Full recovery from the procedure is generally expected within a week. If additional interventions, like stent placement, were done, recovery might take slightly longer. Following the doctor’s advice during this time is crucial for ensuring proper healing and maintaining heart health moving forward.
For many patients, the results of the coronary angiography will guide their long-term treatment plan, which may involve lifestyle changes, medications, or even further procedures like angioplasty. Recovery is not just about physical healing—it’s also about adopting a heart-healthy lifestyle to prevent future issues and keep the arteries clear of blockages.
Is Coronary Angiography Right for You?
Deciding whether a coronary angiography is necessary depends on your specific symptoms, risk factors, and overall heart health. This procedure is most often recommended for individuals who are showing signs of heart disease, such as chest pain, shortness of breath, or abnormal results from other diagnostic tests like stress tests or echocardiograms. However, it may also be used as a preventive measure in certain high-risk individuals, even if they are not yet showing symptoms of coronary artery disease.
Who Should Consider Coronary Angiography?
Several groups of people are prime candidates for a coronary angiogram:
- Patients with Symptoms of Heart Disease: Individuals experiencing persistent chest pain (angina), unexplained shortness of breath, or dizziness may have blocked or narrowed arteries. A coronary angiogram is a valuable tool for diagnosing the underlying cause of these symptoms.
- Those with High-Risk Factors for Heart Disease: People with risk factors such as high cholesterol, high blood pressure, diabetes, or a family history of heart disease are more likely to develop coronary artery disease. A coronary angiogram may be used to detect early blockages before they lead to serious complications like a heart attack.
- Patients with Abnormal Stress Test Results: If a stress test or another non-invasive heart test shows irregularities, a coronary angiogram may be recommended to get a clearer picture of the coronary arteries and assess the severity of the disease.
- Patients Before Heart Surgery: Before undergoing certain heart surgeries, such as valve replacements or bypass surgeries, a coronary angiogram may be performed to evaluate the condition of the coronary arteries and guide the surgical plan.
For these individuals, coronary angiography is an essential diagnostic tool that provides accurate, real-time information about the heart’s blood vessels, helping doctors determine the best course of action. However, it’s not always necessary for everyone. For individuals with a low risk of heart disease, lifestyle changes, medications, and non-invasive tests may be sufficient for managing heart health.
Alternatives to Coronary Angiography
Although coronary angiography is a gold standard for diagnosing coronary artery disease, there are alternative tests that may be used to assess heart health without the need for catheterization. Some of these alternatives include:
- CT Coronary Angiography (CTA): A less invasive form of angiography that uses a CT scanner to create detailed images of the coronary arteries without the need for a catheter. However, it still involves the use of contrast dye and radiation.
- Stress Test: A stress test evaluates how well the heart functions under physical exertion. It is often used as a preliminary test for heart disease, particularly for patients experiencing symptoms like chest pain.
- Echocardiogram: An echocardiogram uses ultrasound technology to create images of the heart and assess its structure and function. It can detect issues like heart valve problems or weakened heart muscles.
- Nuclear Stress Test: Similar to a standard stress test, this test uses a small amount of radioactive material to visualize blood flow to the heart and detect areas that may not be receiving enough oxygen.
Each of these alternatives has its own strengths and limitations, and the choice of test depends on the individual’s symptoms, risk factors, and overall health. While these tests can provide useful information about heart function, they may not offer the same level of detail as a coronary angiogram when it comes to visualizing the coronary arteries and diagnosing blockages.
Ultimately, deciding whether to undergo coronary angiography is a decision best made in consultation with your healthcare provider. Together, you can weigh the risks and benefits of the procedure based on your unique situation, and determine the most appropriate steps for diagnosing and managing your heart health.
FAQ
1. What is coronary angiography?
Coronary angiography is a medical imaging procedure that uses X-ray technology and contrast dye to visualize the coronary arteries, allowing doctors to detect blockages or narrowing in the arteries that could lead to heart disease.
2. Why is coronary angiography performed?
Coronary angiography is performed to diagnose coronary artery disease, assess heart health, and guide treatment decisions for patients with symptoms of heart disease such as chest pain, shortness of breath, or abnormal stress test results.
3. How long does a coronary angiography procedure take?
The procedure typically takes between 30 minutes and an hour, depending on the complexity of the patient’s condition and the number of images required to assess the coronary arteries.
4. Is coronary angiography painful?
No, coronary angiography is generally not painful. Patients are usually awake during the procedure and may feel pressure or mild discomfort at the catheter insertion site, but local anesthesia is used to numb the area.
5. What are the risks associated with coronary angiography?
While the procedure is generally safe, some risks include allergic reactions to the contrast dye, bleeding or bruising at the catheter site, blood vessel damage, and, in rare cases, heart attack or stroke.
6. How do I prepare for coronary angiography?
Before the procedure, you may need to fast for several hours, temporarily stop taking certain medications, and inform your doctor of any allergies, especially to contrast dye or iodine.
7. How long is the recovery after coronary angiography?
Most patients recover quickly and can return home the same day, though it’s recommended to avoid strenuous activities for a few days. Full recovery usually takes about a week.
8. Can coronary angiography detect heart disease early?
Yes, coronary angiography can detect early signs of coronary artery disease by revealing blockages or narrowing in the arteries, which may not yet be causing noticeable symptoms.
9. What are the alternatives to coronary angiography?
Alternatives include CT coronary angiography, stress tests, echocardiograms, and nuclear stress tests, which can provide valuable information about heart health without requiring catheterization.
10. When should I consider coronary angiography?
If you are experiencing symptoms of heart disease, have high risk factors such as high cholesterol or high blood pressure, or have abnormal results from other heart tests, your doctor may recommend coronary angiography to get a clearer picture of your coronary arteries.